*We will be regularly updating this post as the various States and Territories update their processes. Where information is not currently available for the 2026 clinical year we have used information from the previous year, i.e. 2025. If you notice anything incorrect please let us know in the comments below.
It’s time for our well-liked guide on applying for internships in Australia. Wondering how to become an intern in Australia? It’s that time of year when the process of applying for and assigning medical intern positions in Australia gets underway. So, now is the ideal moment to outline the procedure. I managed the largest intern application system in Australia, specifically the NSW Intern application system, for four years. Therefore, I would like to impart some of the insights I gained from that experience to this year’s medical graduates. Wondering how to become an intern in Australia? It’s that time of year when the process of applying for and assigning medical intern positions in Australia gets underway. So, now is the ideal moment to outline the procedure.
Recent Developments of Note.
- One interesting phenomenon of the past few years of internship allocations in Australia has been that most jurisdictions have not been able to fill all intern posts. This theoretically creates more opportunities for IMG doctors. We have attempted to indicate the number of unfilled posts from last year where known.
- Consistent with the move to a 2-year Prevocational Training framework we understand that all jurisdictions are now offering a minimum 2-year contract for Internship.
(Disclaimer: All information here has been sourced in good faith but things do change so you should always do your own due diligence in such matters, we are providing this information to aid you in your application but take no responsibility for any outcomes)
As has been the case in past years the main Intern application and allocation dates are aligned across Australia so that every State and Territory opens and closes their systems at the same time and makes offers at the same times. There are some variations to this in relation to special priority categories in some States and Territories. The key things that all medical graduates should consider in preparing their medical internship application in 2025 year for the 2026 clinical year are as follows:
- Applications open on 6th May 2025.
- Applications close on 5th June 2025.
- Make sure that you have an Intern Placement Number; otherwise, you won’t be able to apply.
- You should research the application requirements now as there may be some “surprises”. As soon as the application system opens, register or log in and ensure that you have everything you need to complete your application.
- Understand where you sit on the priority list for any State or Territory you are applying to.
- If you are required to attend an interview. Ensure you have obtained leave from your medical school requirements to attend.
- Also, consider whether the interview will be in-person, via phone, or video.
- Give yourself time to request referees, assemble a Resume, if required, and find other documents you may need.
- The first National Intern Offer Period commences 14th July 2025.
- Offers for Rural and other Special Pathways will come out starting from 14th July 2025.
- The first offers for all other main pathways will come out from 16th July 2025.
- Generally, you only have 48 hours to accept. So make sure that you have regular access to your email.
- The National Close Date for 2026 Intern Recruitment is 17th October 2025. After which all remaining vacant intern positions move into the Late Vacancy Management Process.
- The National Late Vacancy Management Process closes on 20th March 2025
- Stay in touch with your medical school. you may be worried about completing your degree on time but they are all working very hard with the other institutions to give you the best chance of completion.
Number of Intern Positions Available Across Australia in 2025
last updated 13th April 2025
| Jurisdiction | Intern Numbers 2026 | Intern Numbers 2025 | Intern Numbers 2024 | Population | Interns per 100K Person** | Unfilled Posts 2025 | Annual Salary |
|---|---|---|---|---|---|---|---|
| New South Wales | 1,175 | 1,162 | 1,135.5 | 8,511,200 | 13.8 | 42 | $76,009 |
| Victoria | 973 | 971 | 960.5 | 7,013,000 | 13.9 | 2025 unknown, 16 in 2024 | $85,414 |
| Queensland | 921 | 885 | 862 | 5,608,700 | 16.4 | not available | $90,141 |
| Western Australia | 401# | 401 | 401 | 2,981,800 | 13.5 | not available | $90,864,– $119,165*** |
| South Australia | 353# | 353 | 311 | 1,882,700 | 18.8 | 40 | $81,814 |
| Tasmania | 106# | 106 | 105 | 576,000 | 18.4 | not available | $87,000 |
| Australian Capital Territory | 96# | 96 | 95 | 475,600 | 20.2 | not available | $86,619 |
| Northern Territory | 88 | 88 | 65 | 255,600 | 34.4 | not available | $90,150 |
| Junior Doctor Training Program (Commonwealth) | 115# | 115 | 115 | not available | varies | ||
| TOTAL | 4228 | 4,177 | 4,050 | 27,309,400 | 15.4 |
** From https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release
***If allocated to WA Country Health you will receive a higher payment
#2025 numbers not yet released, PMCWA does not list intern numbers for Western Australia.
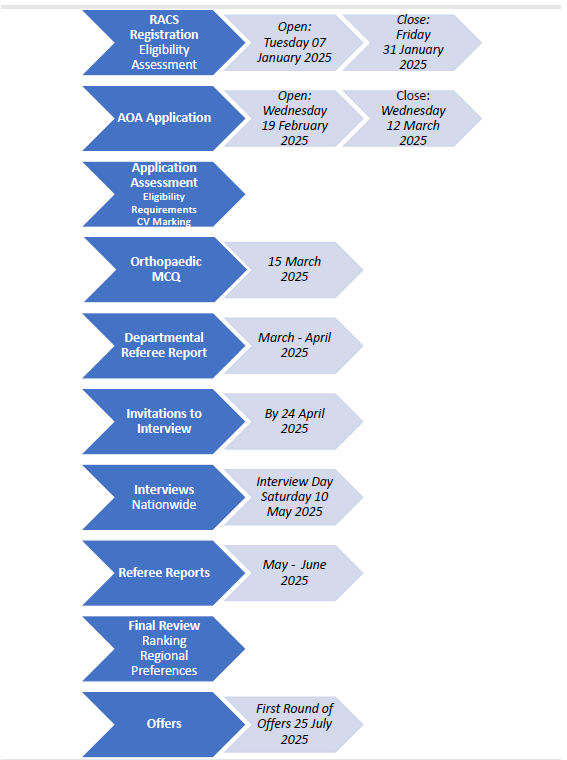
Key Dates for Internship Applications in 2025 and 2026
| Applications Open | Tuesday 6th May 2025 |
| Applications Close | Thursday 5th June 2025 |
| National Offer Period 1 Opens (Rural and Aboriginal and Torres Strait Islander Pathways) | Monday 14th July 2025 |
| National Offer Period 1 – Main Offers | Wednesday 16th July 2025 |
| National Offer Period 1 Closes | Friday 1st August 2025 |
| 1st National Audit of Acceptances and Unplaced Applicants | Tuesday 5th August 2025 |
| National Offer Period 2 Opens | Thursday 14th August 2025 |
| National Offer Period 2 Closes | Friday 5th September 2025 |
| 2nd National Audit of Acceptances and Unplaced Applicants | Tuesday 9th September 2025 |
| National Offer Period 3 Opens | Thursday 18th September 2025 |
| National Offer Period 3 Closes | Friday 17th October 2025 |
| 3rd National Audit of Acceptances and Unplaced Applicants | Tuesday 21st October 2025 |
| National Late Vacancy Management Process Starts | Monday 10th November 2025 |
| National Late Vacancy Management Process Closes | Friday 20th March 2026 |
Tip #1. Your Medical Intern Placement Number.
The IPN is a unique nine-digit number that has been generated by AHPRA and has been provided to medical schools for distribution to all 2025 final-year medical students. The number is used as part of the national audit process (which ensures that intern positions across the country are made available to as many applicants as possible) as well as to streamline registration.
This number is not the same number as your AHPRA registration number or student number. If you have not received your IPN you should check with your school.
If you are not an Australian medical student you won’t be issued an IPN. If you are applying as a non-Australian medical student you do not require an IPN. However, please note that unless you are a New Zealand medical student your chances of gaining an internship are very slim.
Tip #2. Other Things You Will Likely Need to Become an Intern in Australia.
The majority of States and Territories require you to upload an academic transcript as proof that you are indeed a medical student.
They will also request evidence that you satisfactorily meet the AHPRA English Language requirements. This may seem a bit ridiculous given that you have been attending medical school in English for the last 4 or 5 years. But it is the law. So check whether you may need to submit an up-to-date English test result or some other form of documentary evidence such as a high school certificate.
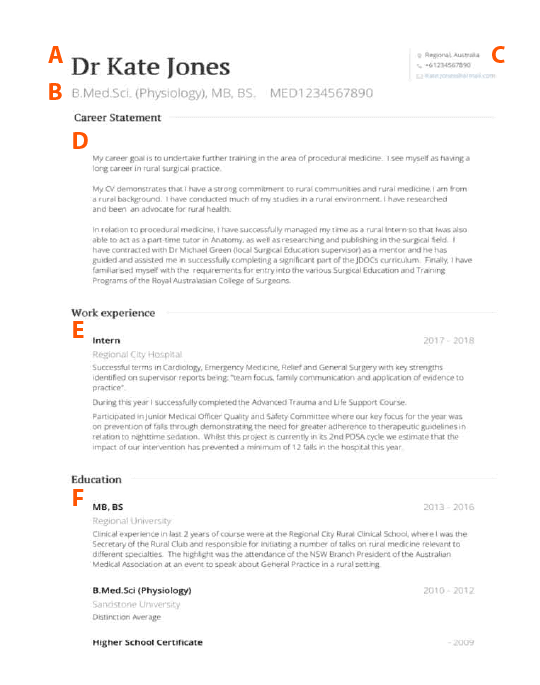
Most States and Territories will also request a CV or Resume. For tips on your CV or Resume see our ultimate guide to CVs or watch a video series about this.
Some States and Territories have a CV template that they suggest that you use to fill in your information. In the case of Victoria, you are no longer required to use the suggested template (change from last year). It’s probably fairly harmless to use the template for the other States and Territories. But if you are thinking about your future career, then now is a good time to be designing your own CV. The risk of using the template is that you don’t stand out from other candidates.
You will need to also provide proof of your identity, citizenship, residency, or visa. And if you have had a name change along the way you will probably also need to provide some documentation in relation to this.
Why All This Information?
The State and Territory bodies who administer the Intern application process have a responsibility to ensure that you are eligible to apply for provisional registration at the end of the year in order to work as an Intern. They collect this information to check that everything is in order so that you are indeed eligible to apply. Employers can get rightly annoyed when told that someone who has been allocated to work with them as an Intern will have a several-month delay whilst they resit an English language test.
However, it’s your responsibility to ensure that you are eligible for registration. So you should also be checking these things yourself.
It’s hard to fathom given the amount of communication from health departments, medical schools and student colleagues. But every year there are a handful of medical students who forget to apply for their internship. This means having to wait another year. Don’t let that be you.
Dr Anthony Llewellyn | Career Doctor
Tip #3. Research and Apply Early.
It’s hard to fathom given the amount of communication from health departments, medical schools, and student colleagues. But every year there are a handful of medical students who forget to apply for their internship. This means having to wait another year. Don’t let that be you.
There are even more students who leave their applications to the last minute. Only to find that they are missing a vital document. For example, this could be evidence you need to substantiate that English is your first language, such as a high school certificate. Or perhaps your last name has changed whilst you have been in medical school? Or maybe you need to submit a CV with your application?
As soon as the application page opens for each State and Territory you are going to apply to make sure you register. And then go as far through the process of applying as possible so you can see if there is some sort of document you need to obtain.
Tip #4. Practice Your Interview Technique, Including Video Interview Technique.
As part of your application to become and Intern in Australia you may need to undertake an interview. This could take the form of a faced to face interview or a video interview. The COVID pandemic resulted in a shift to a preference for video interviewing job applicants in Medicine in Australia. Many employers now see an inherent advantage to this. So you should still be prepared for the fact that this year your interview may be conducted on video.
There’s a lot more than you think to video interviewing. For a rundown on this check out this post.
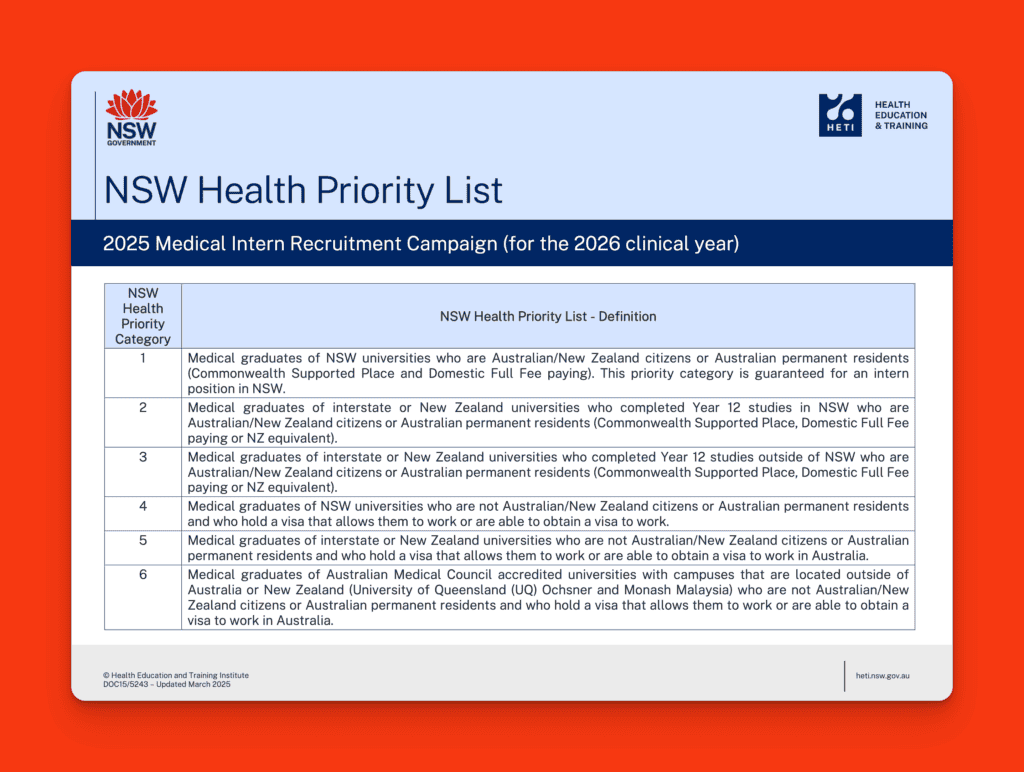
Tip #5. Know Where You Sit In The Priority List.
Its important to know where you sit on the priority list. Each State and Territory has a slightly different order but in essence, it goes something like this:
- If you are an Australian Citizen or Permanent Resident and went to Medical School in that State or Territory you are top of the list.
- If you are an Australian Citizen or Permanent Resident and went to Medical School in another State or Territory or New Zealand you are probably second.
- If you are an international student who studied Medicine in Australia you are probably next.
Tip #6. Know the Key Dates, including Offer Dates.
As noted above it’s crucial that you know the key dates. If you miss your application submission date (and it does happen) there is no allowance for a last-minute submission. You also need to make sure you are available to accept your offer. Generally, the window for offer acceptances is quite narrow (often 48 hours).
For this year the day on which the first round of offers can be made nationally is 14th July 2025 for the rural and other special pathways. The first date that offers can be made to the main group of applicants is 16th July 2025 and most offers will come out on that day. Thereafter there is a series of offer windows for 2nd and 3rd round. In between which there is a mandated pause, which allows the National Intern Audit process to run. This is a system that works to ensure that vacancies are being freed up as soon as possible by highlighting medical students who may have an offer in more than one jurisdiction and ensuring that they accept one offer and decline others.
The nationally coordinated offer system concludes on 17th October 2025. Technically this is the last date that the Medical Board can guarantee that they will be able to process your registration application in order for you to commence your internship on time the following year in 2026.
However, there are generally still vacancies after this point and so the National Intern Audit Office switches over to an ad hoc coordinated late vacancy management process from 10th November 2025. This runs up until 20th March 2026, which is around the 1st term to 2nd term changeover for most interns. So it is still possible to commence your internship in 2026 but you might have to finish one or two terms in the following year.
The National Intern Audit.
States and territories share intern applicant information at pre-agreed dates. This data is then used to identify applicants who have applied for and/or accepted intern positions in more than one state/territory. Applicants who have accepted more than one intern position will be contacted by the National Audit Data Manager by phone or email and given 48 hours to withdraw from all intern positions, except the one where they intend to undertake their intern year.
If you don’t respond to the National Audit Data Manager and/or do not withdraw from all positions except one, the relevant states/territories where you have accepted an offer will be advised and all offers, except for the first offer you received may be withdrawn.
The Late Vacancy Management Process.
The Late Vacancy Management (LVM) Process runs from Monday 10th November 2025 to Friday 20th March 2026. The process ensures any late vacancies are offered to eligible intern applicants who have not yet accepted an internship position.
The Late Vacancy Management Process is coordinated by the National Audit Data Manager on behalf of states and territories. So you should ensure you have updated your contact details if you are going overseas during the Late Vacancy Management Process period.
The National Audit Data Manager will send out emails to participants who will need to opt into the Late Vacancy Management Process if they still wish to receive an offer to be an Intern in Australia.
If an applicant does not respond to this email, they will no longer be eligible to receive an internship offer, and their application will no longer be considered in any Australian jurisdictions.
The process is open to medical graduates of AMC-accredited medical schools who have applied for and are not holding a 2026 intern position through the Commonwealth or states and territories at the National Close Date for Intern Recruitment. Participation in the LVM is an opt in process – you must confirm that you want to participate in the LVM by responding to the National Audit Data Manager by e-mail.
Priorities Within Priorities.
Some States and Territories also have priority pathways to ensure that groups such as Aboriginal and Torres Strait Islanders and doctors who wish to work rurally or regionally can obtain their preferred placement early.
So if you are an International student and like the idea of working rurally, it’s probably a good idea to consider a rural pathway as it will likely boost your chances of gaining an Intern position earlier in the process.
Further Information on Each Jurisdiction
New South Wales

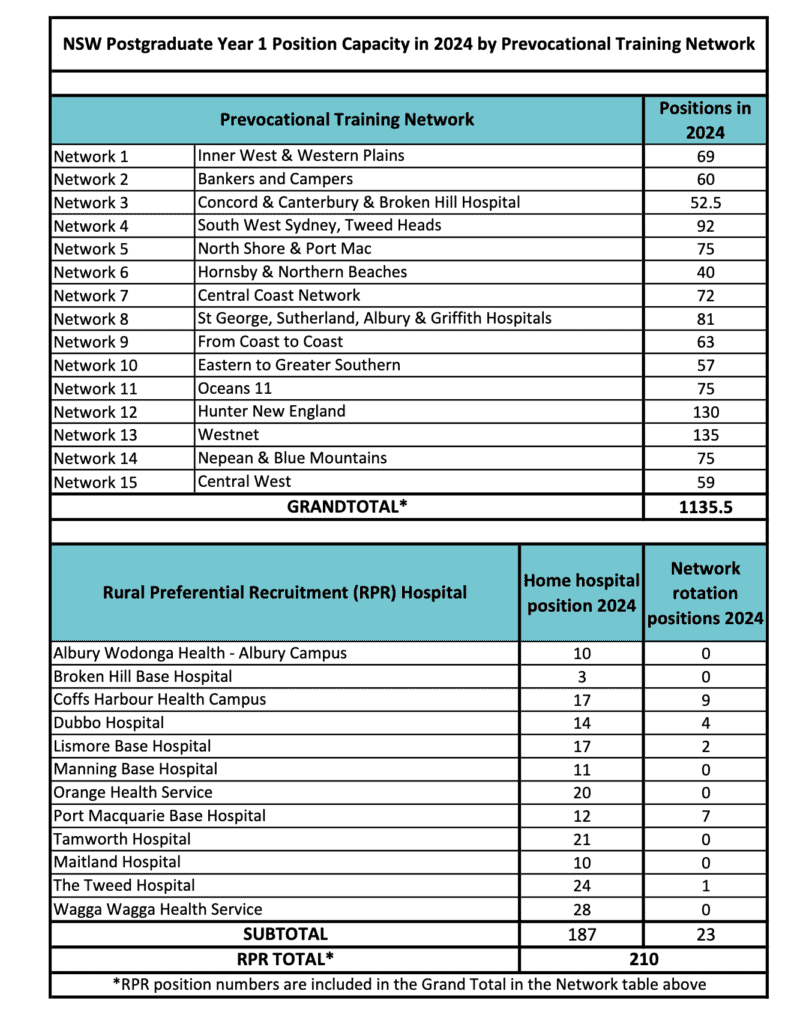
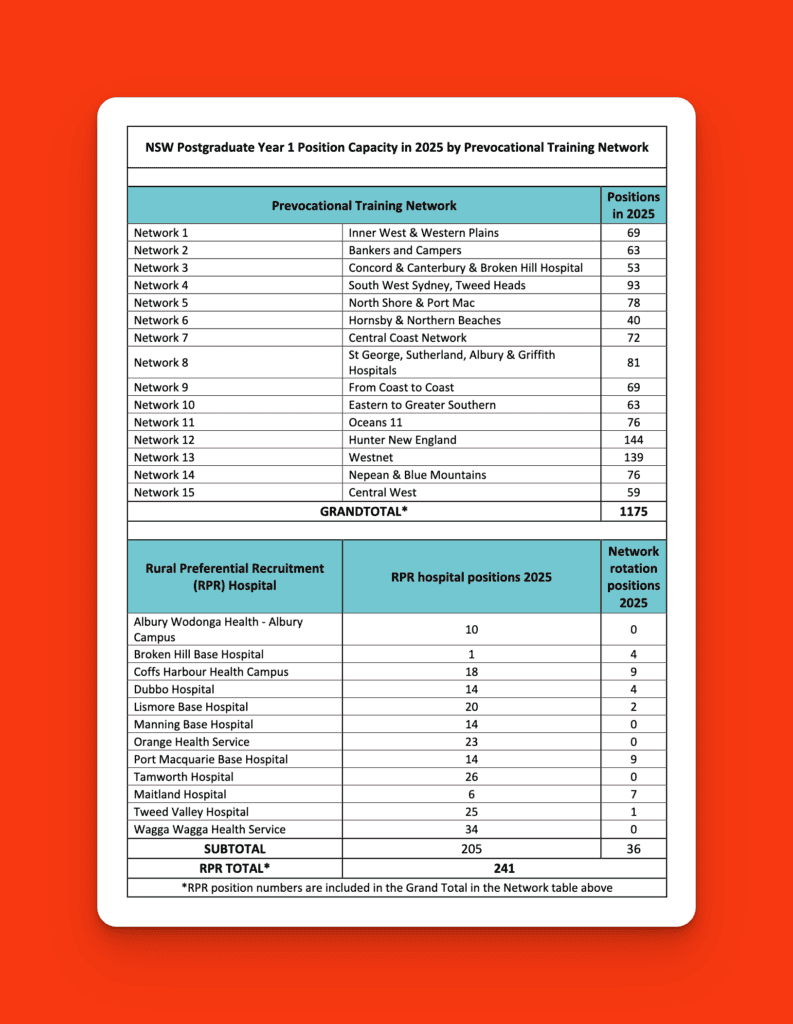
Intern Positions = 1,175 (including 241 rural preferential) across 15 Networks
Unfilled posts in 2025 = 42
Annual Salary = $76,009
Length of Contract = normally 2 years
Professional Development Allowance = nil
The 4 Pathways in NSW
You have the option of applying through one of 4 pathways:
– Aboriginal Recruitment Pathway
– Rural Preferential Pathway
– Regional Allocation Pathway
– Optimised (or Main) Pathway
Only applicants who go through the Rural Preferential Pathway need to submit a CV and attend an interview. All other pathways are based on applications only. A key advantage of the Aboriginal, Rural, and Regional Allocation Pathways is that you are far more likely to be given your preferred hospital network.
Can You Stack or Hack the HETI Optimised Pathway?
Each year the question comes up. Is it possible to hack or game the HETI optimised pathway. If you search enough you will find various reddit threads or blog posts covering this topic by authors purporting to have much greater understanding of mathematics than this author.
The posts give an outline of how the HETI allocation algorithm works. The algorithm incorporates an annealing component with the purpose of optimizing the outcomes for as many applicants as possible. Hence the name “Optimised Pathway”. It does this not necessarily by allocating everyone to their most preferred network but by attempting to allocate as many people as possible to a higher preference network, therefore, guaranteeing that more applicants get a 1st or 2nd or 3rd preference overall.
The general gist of the blogs written about hacking the HEIT algorithm is that if you are super keen on a certain NSW network. Let’s call this Network A then you should attempt to put this as your highest preference and then load all of your next higher preferences with networks that are not as popular.
You can probably already see how this tactic can backfire massively for you.
There’s a couple of things that can go wrong here.
First algorithm is more likely to identify you as one of those few applicants that prefer the unpopular Network Z and allocate you there, thereby satisfying the aims of the algorithm.
Second, you will be stacking your preferences based on historical data that does not reflect the desires of the current applicant cohort.
And third, if large number of applicants does the same thing then you are probably all going to advantage those applicants that just put down the networks in their actual order of preference.
Take home message. Don’t try to stack or hack the HETI algorithm.
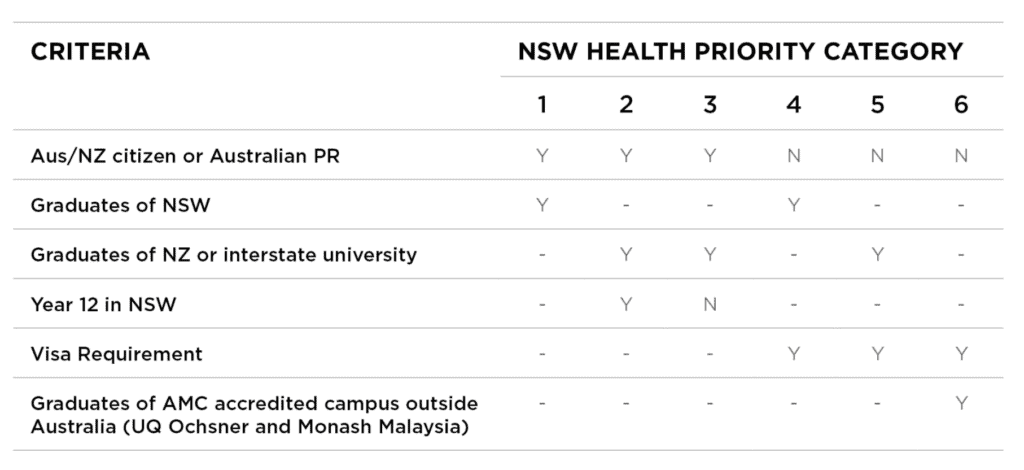
Intern Placement Priorities in NSW:
Victoria

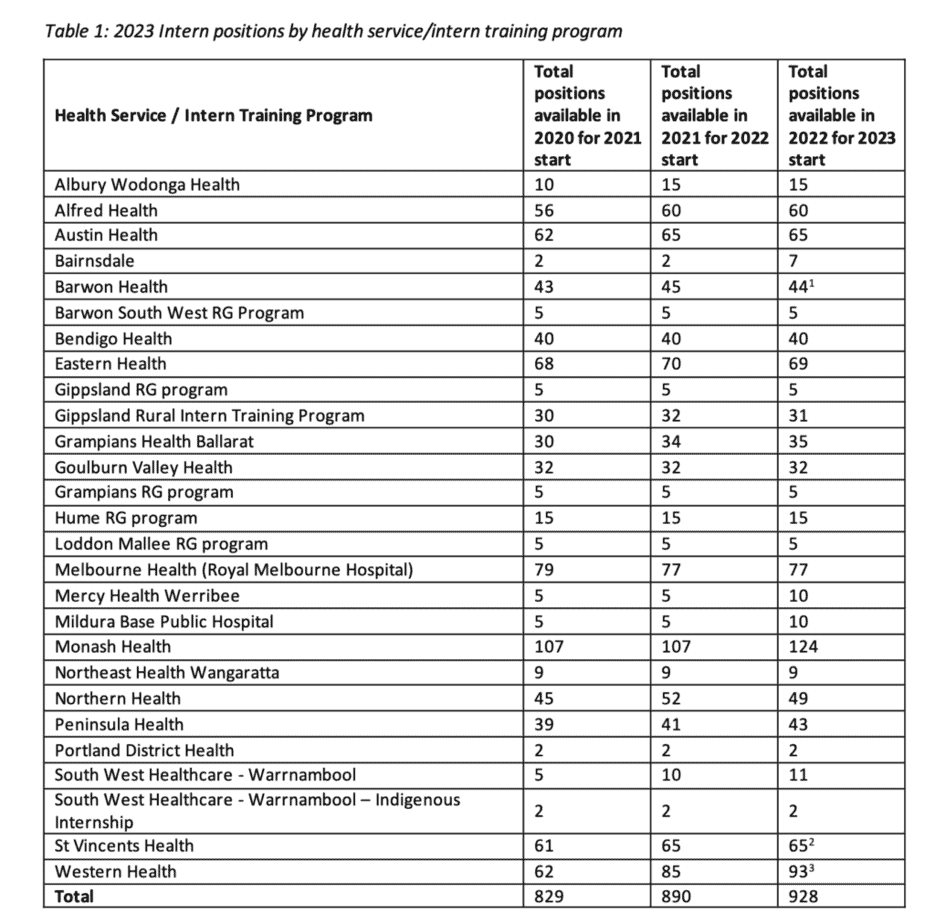
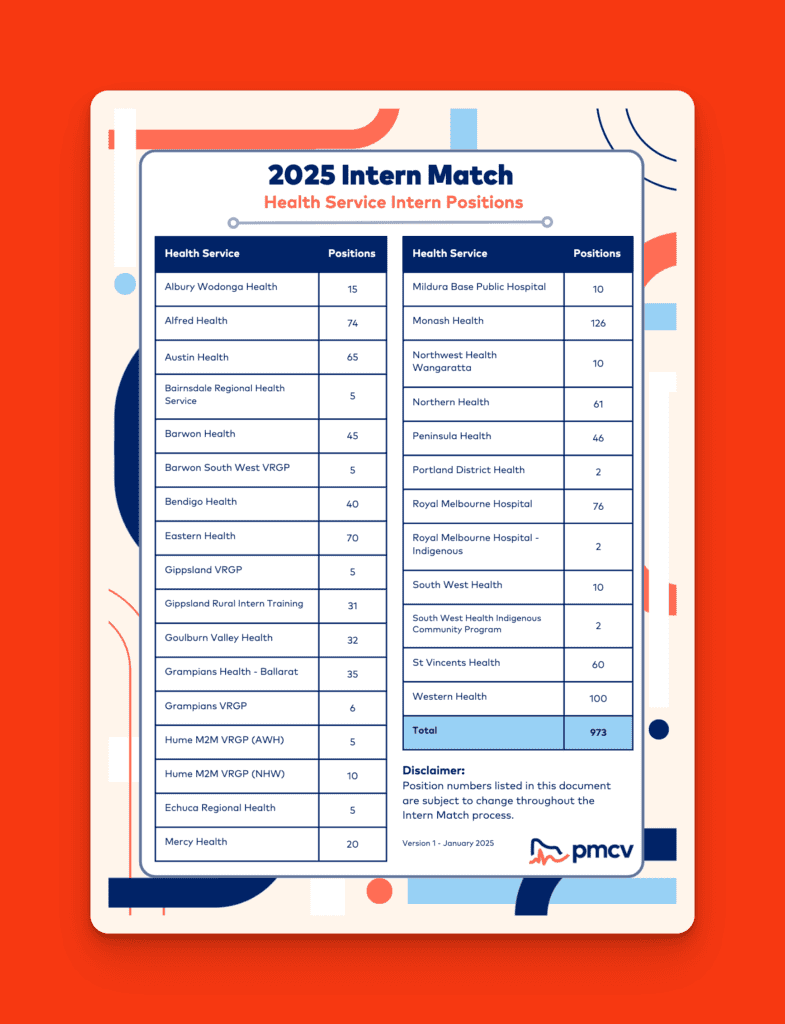
Intern Numbers = 973 (includes an unspecified number of Rural Preferential posts)
Unfilled Positions in 2025 = unknown (2024 was 16)
Annual Salary = $85,414
Length of Contract = 2 years
Professional Development Allowance = $3,888 per annum
c/- PMCV
Internship in Victoria works around a computer matching system that the Postgraduate Medical Council of Victoria administers.
The Allocation & Placement Service is a mathematical process that matches the preferences of both candidates and Health Services and is designed to be “impartial and transparent”.
Candidates create an account and then register with the Intern match. The second step is to select your preferred services. At the same time, the health services also place preferences. The matching process of successful candidates to positions according to rankings.
For Victoria, you will need to submit referees as well as a CV. In past years this had to be on the quite unattractive PMCV standardised CV Template. The status of this template has now been downgraded to a “guide”. You don’t have to put a photo on your CV. I would recommend using your own CV template and not include a photo.
Pre Recorded Video Interviews
In 2020, Victorian Health Services began the use of video-recorded interviews. This continues for 2025 for certain candidates. The system appears to be being used as an efficient way for certain services or hospitals to review applications without arranging formal interview panel days and for candidates to appear in person.
All VRPA applicants and all VIA Group 4 applicants will be required to complete a video interview.
The way these interviews work because you are usually allocated a specific time to log into the system. Once you have gone through a couple of orientation steps you are usually given a series of questions and asked to record your answers. Generally, you don’t get a second go if you are not happy and the time is limited. It is vital therefore that you practice before you do your interview and ensure you have optimised your video environment.
You are able to complete your recording at any time during the specified video interview period. All candidates are required to answer 3 questions. Questions are randomly selected from 3 different question banks. There is one additional question if you are applying for the Regional Pathway.
Response times are 2 minutes per question. You get one minute to read the question and prepare your answer before recording.
All health services can use these recordings to rate you along with your CV and referee reports.
Metro hospitals may conduct live interviews with shortlisted candidates at any time before 3 July. Although I understand many do not and just rely on the candidates’ CV, referees and video interviews.
Interns can be allocated to one of 22 hospitals and networks. This includes a small number of community-based internships where the focus is more on community-based models of care, including working in primary care and smaller hospitals.
You can elect to be prioritised for an internship by entering the Victorian Rural Preferential Allocation (VRPA) match. Where you can be allocated to one of 5 rurally based networks. This pathway involves a live interview. First-round offers for VRPA come out on 18th July on the national rural allocation date.
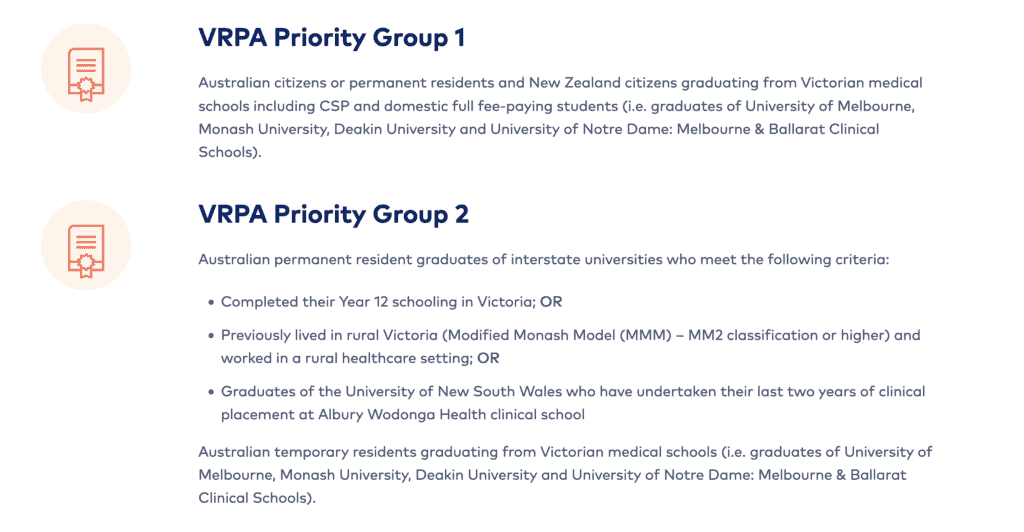
Intern Placement Priorities in Victoria
Intern placement priorities have altered for 2025 with the introduction of a 3rd priorty group for the Victorian Rural Preferential Application (VRPA) pathway and renaming the main pathway to the Victorian Interns Allocatin (VIA) pathway with the creation of an additional fourth category for this pathway.
VRPA Priority Group 1 – Graduates from an Australian University identifying as Aboriginal or Torre Strait Islander. Australian Citizen or permanent resident and New Zealand citizens graduating from a Victorian Medical School.
VRPA Priority Group 2 – Australian Temporary residents graduating from a Victorian University. Graduates of the University of New South Wales who have undertaken their last two years of clinical placement at Albury Wodonga clinical School. Australian Citizen or permanent resident and New Zealand citizens graduating from an interstate Medical School but completed year 12 in Victoria. Completed their Year 12 schooling in Victoria; OR Previously lived in rural Victoria (Modified Monash Model (MMM)1 – MM2 classification or higher) and worked in a rural healthcare setting; OR Graduates of the University of New South Wales who have undertaken their last two years of clinical placement at Albury Wodonga Health clinical school.
VRPA Priority Group 3 – Australian citizen or permanent resident or New Zealand citizen graduating from an interstate or New Zealand University. Australian Temporary resident graduating from an interstate
University.
VIA Group 1 – Graduates from an Australian University identifying as Aboriginal or Torre Strait Islander. Australian Citizen or permanent resident and New Zealand citizens graduating from a Victorian Medical School.
VIA Group 2 – Australian Temporary residents graduating from a Victorian University. Australian citizens or permanent residents and New Zealand citizens graduating from an interstate University who completed their year 12 schooling in Victoria
VIA Group 3 – Australian citizens or permanent residents and New Zealand citizens graduating from an interstate or New Zealand University. Australian Temporary residents graduating from an interstate
University. New Zealand temporary resident graduating from a New Zealand University.
VIA Group 4 – Graduates from and overseas campus of an Australian/New Zealand University accredited by the Australian Medical Council (i.e. Monash University, Malaysia or Ochsner).
Indigenous Internships
Both South West Health Care (based on Warnambool) and Melbourne Health have a small number of Internships reserved for Indigenous graduates.
The Victorian Rural Medical Scholarship Scheme
The Victorian Rural Medical Scholarship (VRMS) supports career pathways to rural medical practice and assists rural and regional health services to attract, employ and retain medical graduates. The VRMS supports medical students with a commitment to working in rural and regional Victoria by providing financial assistance towards living and tertiary expenses in the final year of their medical degree and into their rural intern year.
The VRMS is administered by the PMCV on behalf of the Department of Health of Victoria. Scholarships valued at $20,000 each are available to be
awarded to final year medical students in Victoria. Scholarship recipients are required to commit to a two- year return of service in rural or regional Victoria (within three years from graduating from medical school).
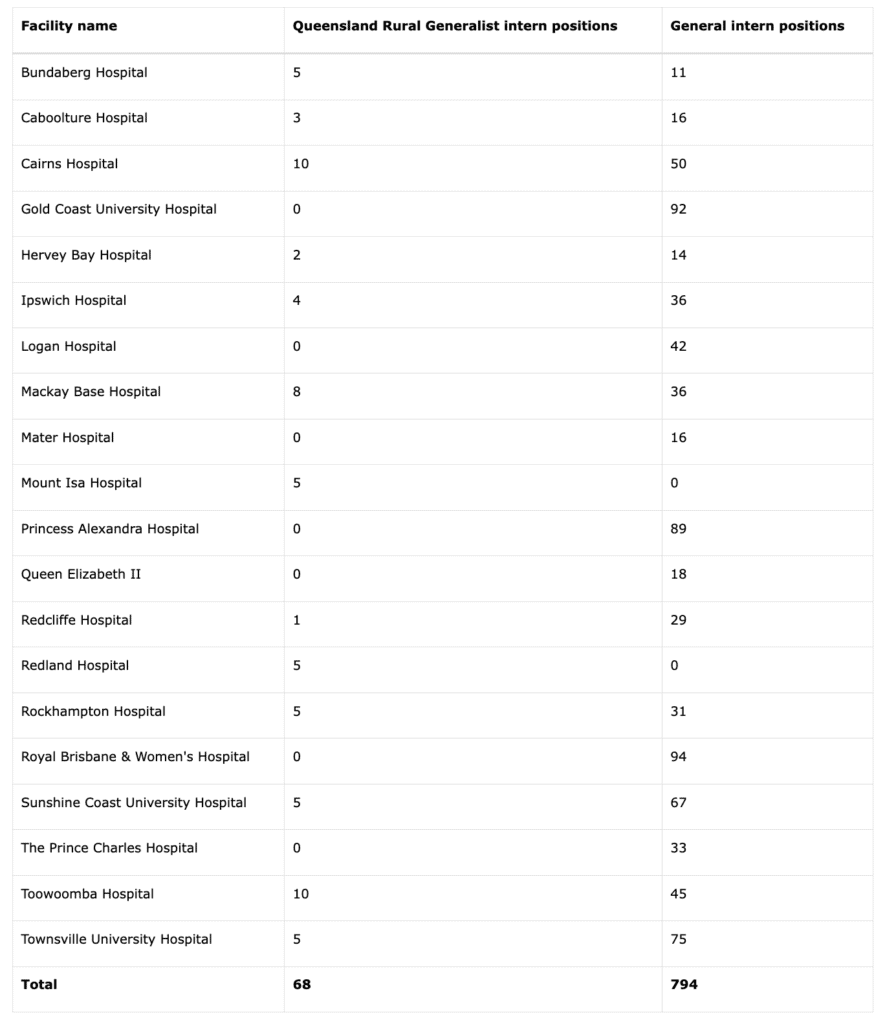
Queensland

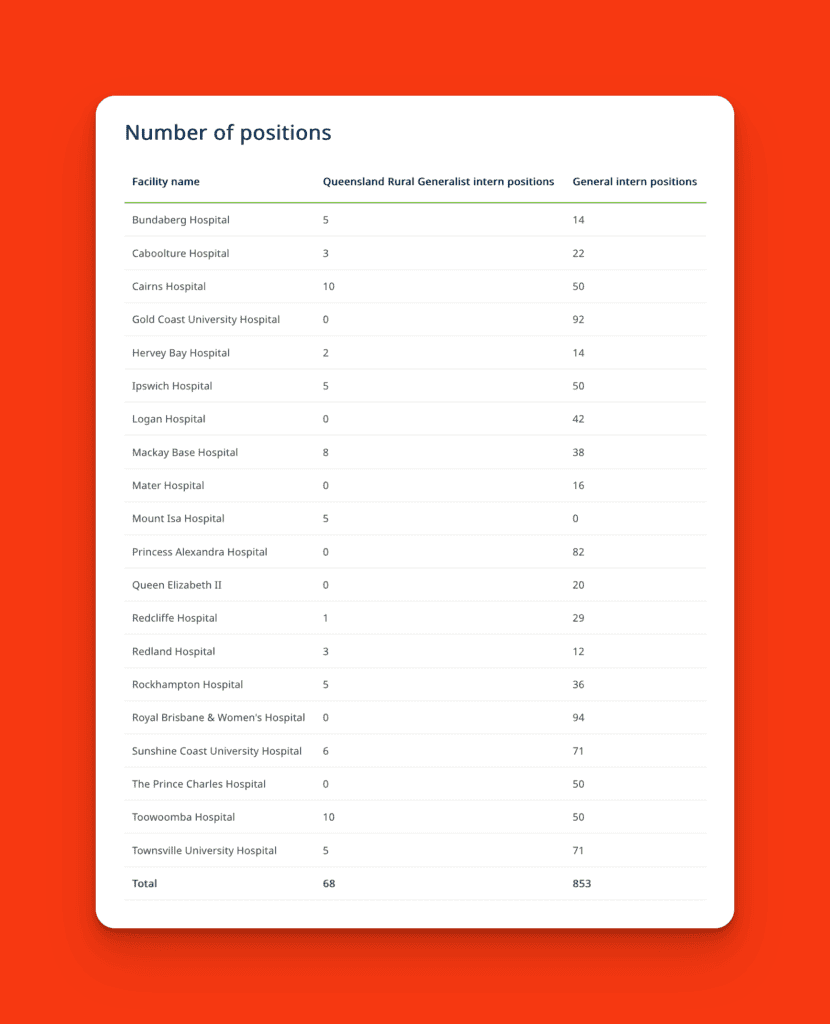
Intern Numbers = 921 (including 68 rural generalist intern positions)
Annual Salary = $90,141
Length of Contract = 1 year
Professional Development Allowance = nil for Interns but $2,640 for RMOs
Queensland has possibly the most complex internal allocation system of all jurisdictions. With a number of pathways and a combination of allocating certain priority groups and merit selection for others.
The Queensland Department of Health coordinates the annual campaign to recruit interns for positions in Hospital and Health Services across the state. There is only one method of application for the intern campaign – the lodgement of an online form via a central application portal.
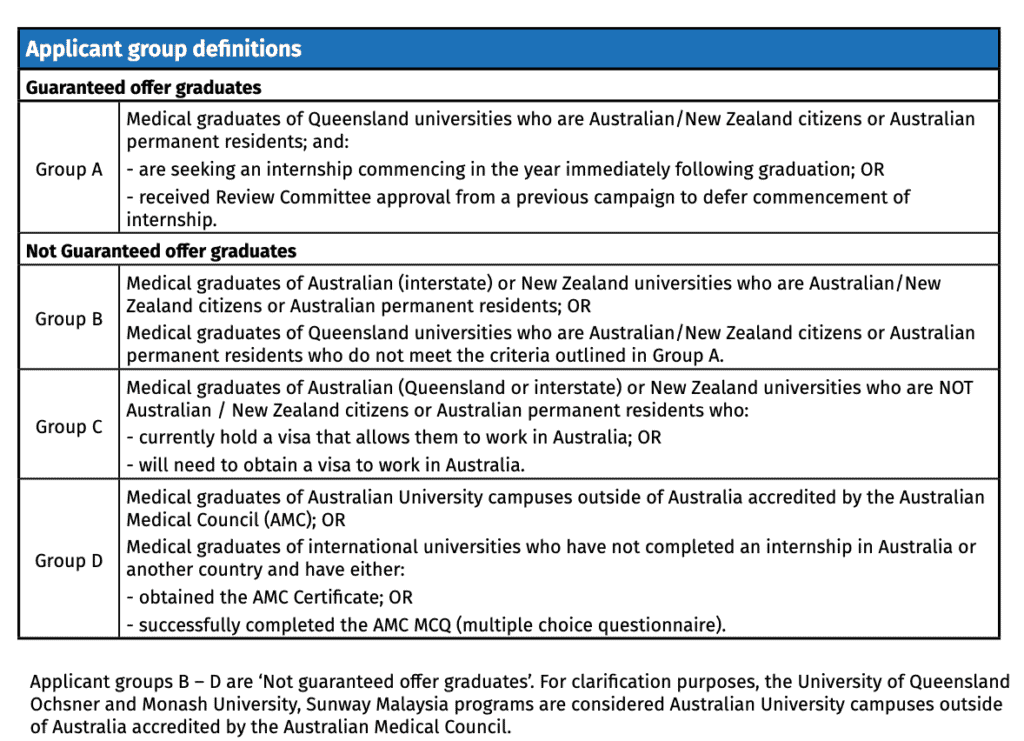
Graduates assign a preference to all participating hospitals from highest to lowest (number 1 being the most preferred hospital). From the applications received via the campaign, graduates are either directly allocated to an intern position determined by their preferences (Group A) or will participate in a suitability assessment process conducted by participating hospitals with remaining intern vacancies (Applicant Groups B-D).
The online portal is used for both the General intern campaign applications and the Queensland Rural Generalist Pathway (QRGP pathway). Applications for the QRGP are submitted first (usually in early March), followed by the General campaign (usually in May).
So, by the time you are reading this post, if you were thinking of applying for the Queensland Rural Generalist Pathway you have missed your opportunity for 2026.
Interns can be allocated to one of 20 Employment Hospitals.
c/- Queensland Health
Applicant Categories
In Queensland, intern applicants are classified into two categories:
Guaranteed offer graduates – Medical graduates who are guaranteed an offer of an intern position in Queensland within their immediate postgraduate year. Allocation to an intern position may be automatic or via random ballot, based on hospital preferences nominated by the individual in their intern application form. (For eligible applicants – see Group A).
Not guaranteed offer graduates – Medical graduates who are not guaranteed an intern offer. A suitability assessment process is undertaken to determine if an offer of an intern position will be made. (For eligible applicants – see Groups B-D). There is no inherent prioritisation across applicant groups, the categorisation of groups are used for reporting for the intern campaign. Each participating Hospital and Health Service establishes suitability assessment processes to recruit from their available applicant pool and are not obligated to sequentially select through the applicant groups. Applicants who do not meet the outlined criteria for Groups A, B, C or D may be considered at the discretion of each participating hospital.
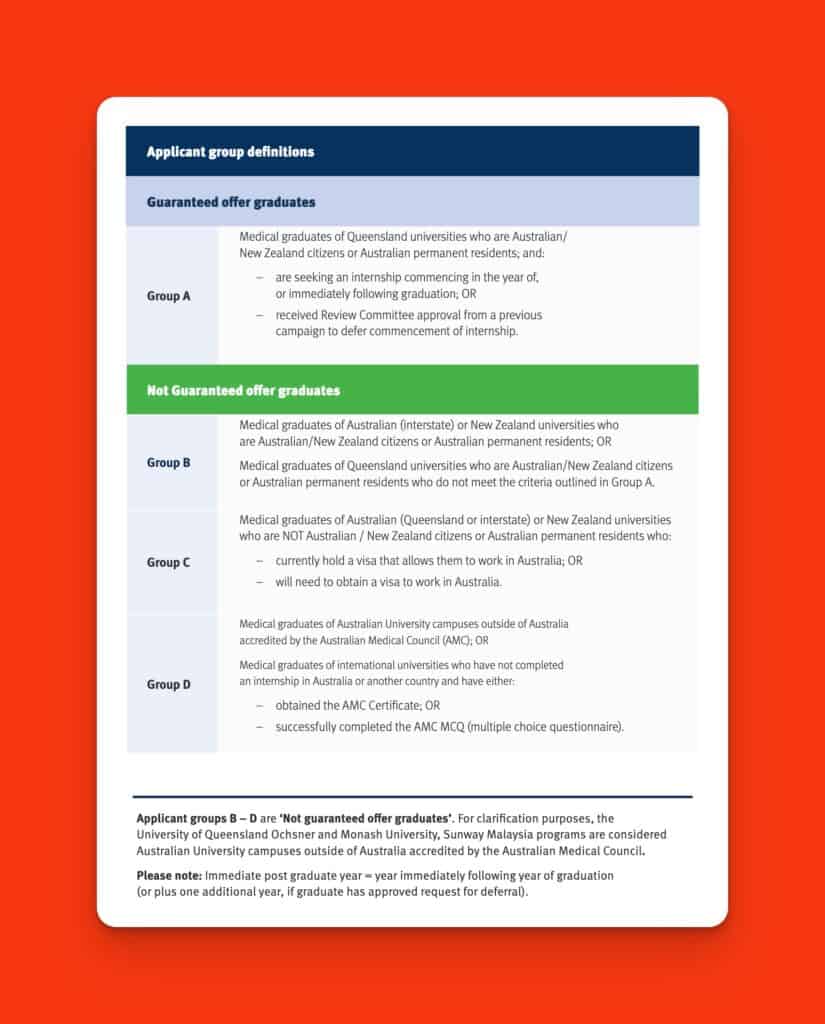
c/- Queensland Health
Note: Queensland is one of the few jurisdictions that offer an opportunity for IMG doctors to complete an internship in Australia. The number of doctors who are successful in doing so each year is rarely more than a handful.
Internship pathways
There are 4 pathways for Intern Allocation in Queensland.
- The Rural Generalist Program offers an opportunity to select a rural hospital centre as part of a program that is a pathway to working as a Rural GP. Applications open 4th March and close extremely early (18th March) for this pathway.
- Aboriginal and Torres Strait Islander Intern Allocation Initiative. The purpose of the initiative is “to promote the success of Aboriginal and Torres Strait Islander medical graduates in the Queensland Health workforce”. Eligible applicants can apply to the Aboriginal and Torres Strait Islander Intern Allocation Initiative to be allocated to their first preferenced hospital. Applications are reviewed by a panel that includes Aboriginal and Torres Strait Islander representation. Applicants who have been confirmed as eligible by the panel will be exempt from the ballot process and allocated to the facility nominated as first preference in their intern application.
- The General Intern Campaign. Which is a ballot process for all category A applicants.
- Suitability assessment for applicants in Group B-D.
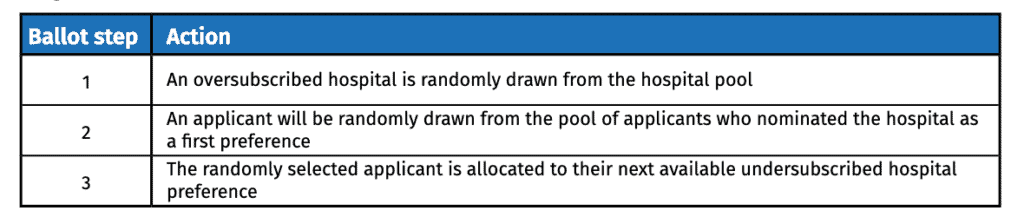
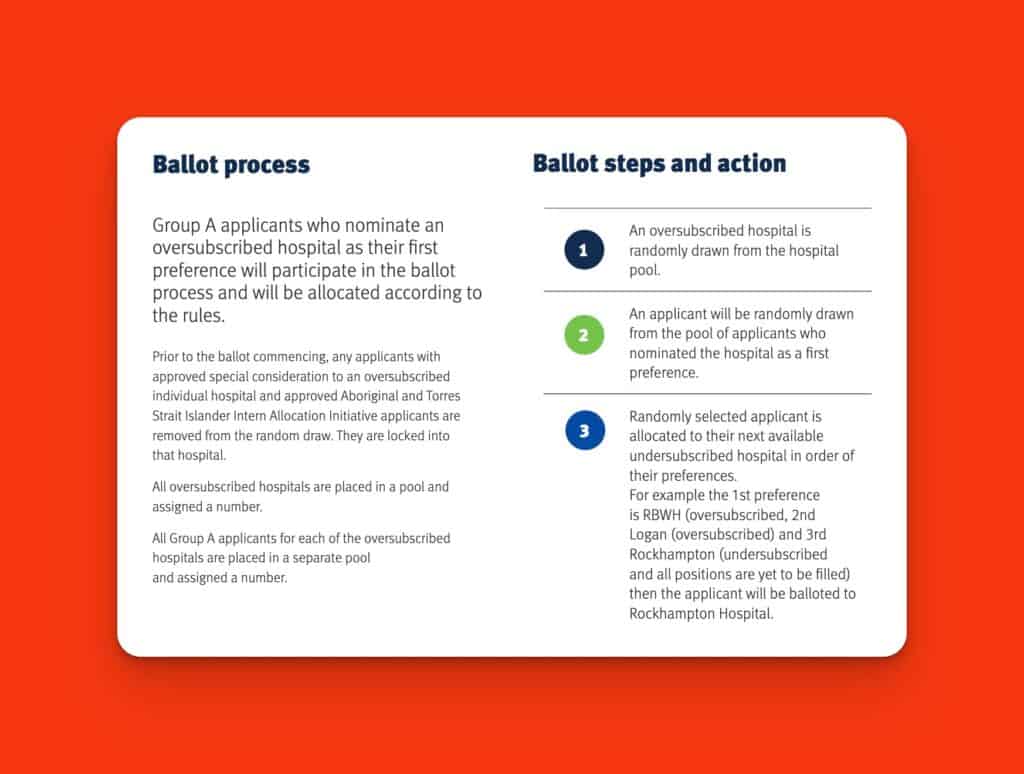
The General Intern Campaign Allocation Process.
After the application period has closed, applications are sorted according to their applicant groups, preferences, and available positions at each facility.
Prior to the ballot taking place a Review Committee considers applications for:
- requests for special considerations
- exemption requests
- joint ticket applications
- deferral requests
After this the ballot commences.
c/- Queensland Health
Applicant Group A candidates who nominate an undersubscribed’ or equal in numbers hospital as first preference will automatically be allocated to that facility.
Applicant Group A candidates who nominate an ‘oversubscribed’ hospital as their first preference may be allocated to another facility via the ballot process.
Merit Selection for Groups B-D.
There is no inherent prioritisation across applicant groups, the categorisation of these groups are used for reporting for the intern campaign. Each participating Hospital and Health Service establishes individual assessment processes to merit select from their available applicant pool and are not obligated to sequentially select through the applicant groups. Applicants who do not meet the outlined criteria for Groups A, B, C or D may be considered at the discretion of each participating hospital.
Following the completion of first-round offers, the Position Status Report (PSR) is updated.
This is an updated list of available positions remaining.
Applicant group B-D candidates have 48 hours to change their preferences if they wish to.
Queensland Health hospitals then assess applications and conduct their own meritorious selection processes. You should contact each Hospital and Health Service directly to find out what they look for in an intern.
If vacancies become available after the First and Second Round offers, individual hospitals will meritoriously select from the remaining applicants for available vacancies. Recruitment to fill available vacancies will continue until the national closing date for intern recruitment. After the closing date, any further vacancies that arise will be filled via the Late Vacancy Management Process (LVMP).
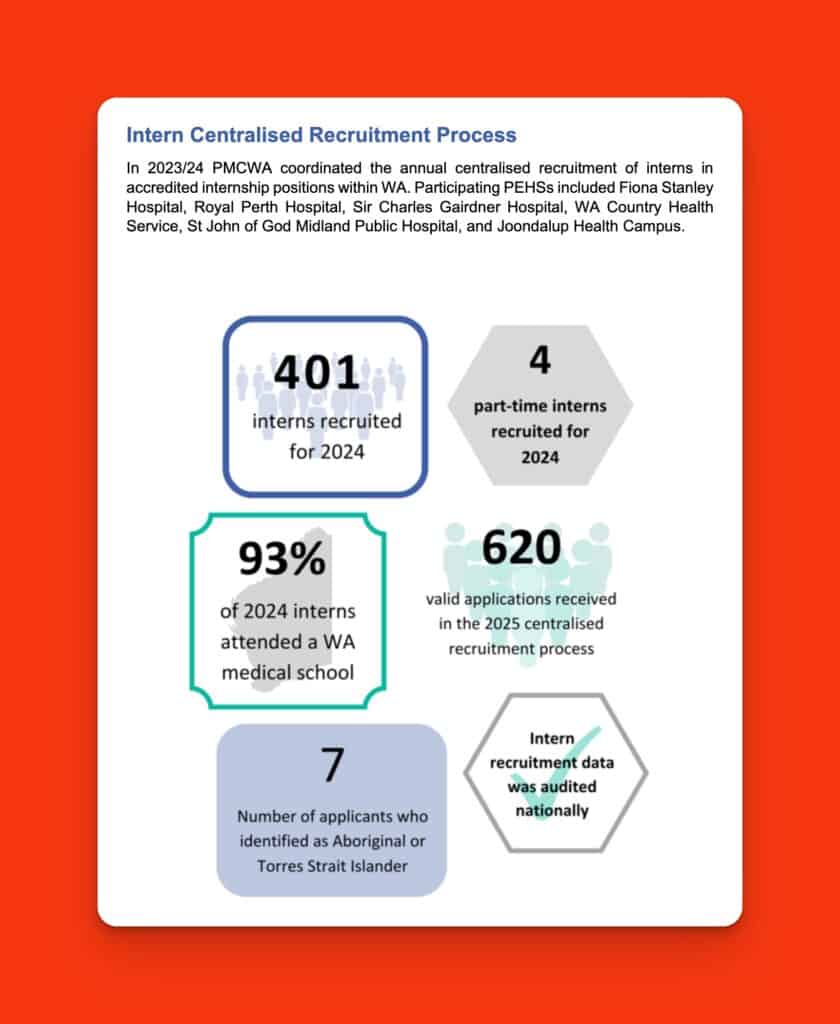
Western Australia

WA Health and the PMC of WA have previously indicated that they can not make Intern numbers available, as these are subject to confirmation by the Primary Employing Health Services.
Estimated Numbers ≅ 401 including 25 Country Health places (based on 2023/2024 PMCWA Annual Report)
Annual Salary = $90,864 ($119,165 if working for Country Health)
Length of Contract = 3 years (in most cases, St John of God Midland = 2 years) with the ability to transfer to a different PEH if all internship requirements are met (IMGs may have shorter contracts tied to their visa status)
Professional Development Allowance = $6,503
c/- PMCWA
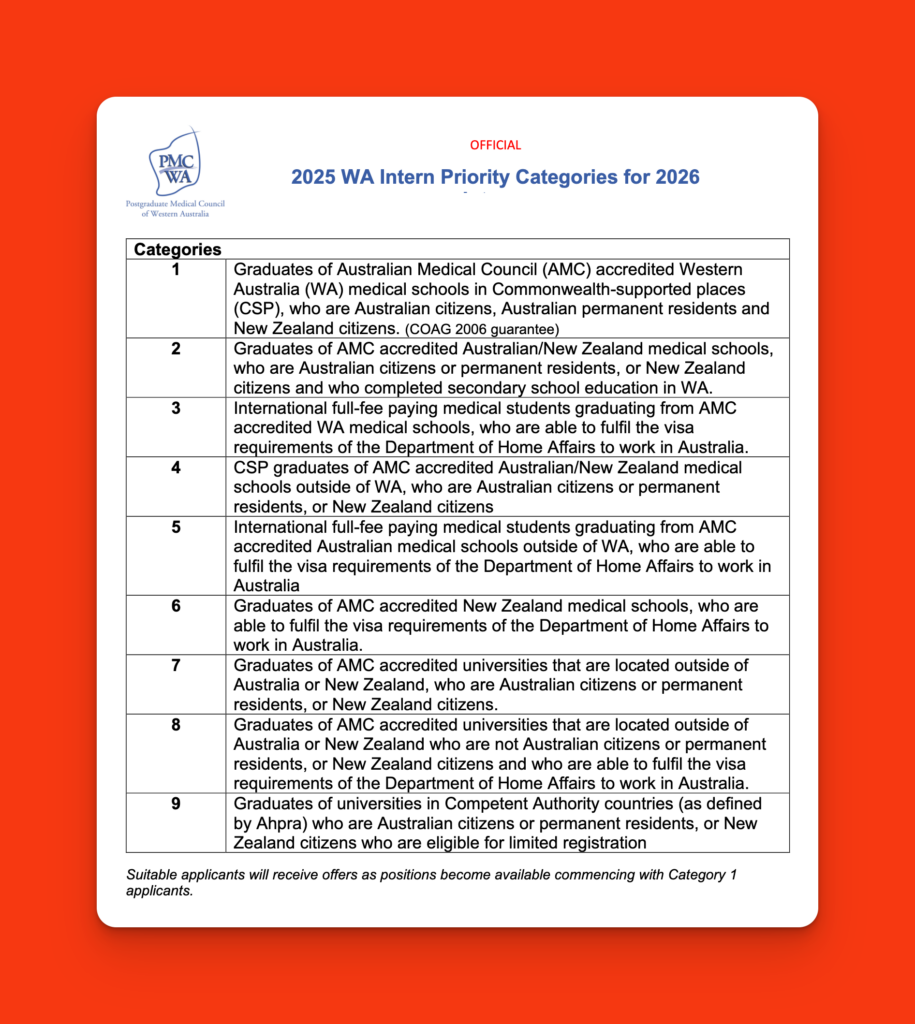
Western Australia Intern Eligibility and Priorities
In Western Australia applications that meet all eligibility criteria, and all essential criteria are included in the suitable recruitment pool. Once in the suitable pool, selection and recruitment decisions are made by the primary employing hospitals.
As with all other Australian jurisdictions, priority is given to Commonwealth funded medical students graduating from Western Australia. This is then followed by Western Australians graduating from interstate universities who want to return to WA; international medical students graduating from WA medical schools; then graduates from other jurisdictions (other than WA). The priority then shifts to international medical graduates from outside of Australia.
Most notably, Western Australia has a final Category, Category 9, for graduates of universities in Competent Authority countries (as defined by Ahpra) who are Australian citizens or permanent residents, or New
Zealand citizens who are eligible for limited registration. Presumably this is to permit Australian students who choose to study in countries such as the UK or Ireland to commence their internship in Australia. How they qualify for this is unclear, as technically, without any overseas experience they are not eligible for the Competent Authority pathway. It appears that they would have to sit and pass the AMC Part 1. Practically this probably means taking a risk and sitting out internship for 6 months to a year, because you can only sit the AMC Part 1 after you graduate from medical school.
c/- PMCWA
Vacancies arise as offers are declined throughout the process, and these vacancies fluctuate each year and will affect how many students outside of WA are offered an intern position.
Western Australia is one of the few options for IMGs to do an Internship in Australia, although as you can see from the above, it is quite limited.
In WA all interns are employed by a Primary Employing Health Service (PEHS).
In WA all interns are employed by a Primary Employing Health Service (PEHS) accredited by PMCWA. Each PEHS is a major tertiary hospital in WA which has been accredited to directly employ interns and provide a high quality intern training program.
The six PEHSs in WA are:
- Fiona Stanley Fremantle Hospitals Group (Fiona Stanley Hospital). Contact: fsh.meu@health.wa.gov.au
- Joondalup Health Campus.
Contact: pgme.jhc@ramsayhealth.com.au - Royal Perth Bentley Group (Royal Perth Hospital).
Contact: rph.pgme@health.wa.gov.au
- Sir Charles Gairdner Osborne Park Health Care Group (Sir Charles Gairdner Hospital). Contact: scgh.postgradmedicaleducation@health.wa.gov.au
- St John of God Health Care (St John of God Midland Public Hospital). Contact: MI.PGME@sjog.org.au
- WA Country Health Service. Contact: meu@health.wa.gov.au
All six WA Health PEHS recruit through the Centralised Intern Application Process. Each PEHS holds an information session during the application period, with presentations from the Medical Education teams, current interns and more.
Following the close of applications in the centralised application process, PMCWA reviews all applications and creates a pool for all suitable applications. Applications appointed to the pool are grouped and managed according to the applicable priority category. As positions become available and selection processes are completed, applicants will be offered positions according to category.
Each PEHS is a major tertiary hospital in WA that has been accredited to directly employ interns and provide an intern training program.
| Employing Health Service | Metro Placements | Rural Placements |
| Fiona Stanley Fremantle Hospitals Group (Fiona Stanley Hospital) | Fiona Stanley Hospital Fremantle Hospital Rockingham General Hospital | Albany Health Service Broome Regional Hospital Northam Health Service |
| Joondalup Health Campus | Joondalup Health Campus | Kalgoorlie Regional Hospital |
| Royal Perth Bentley Group (Royal Perth Hospital) | Royal Perth Hospital Armadale Health Service Bentley Hospital Osborne Park (Women and Newborn Service) Perth Children’s Hospital | Bunbury Hospital Hedland Health Campus Kalgoorlie Regional Hospital |
| Sir Charles Gairdner Osborne Park Health Care Group (Sir Charles Gairdner Hospital) | Sir Charles Gairdner Hospital Graylands Hospital Hollywood Private Hospital Joondalup Health Campus Osborne Park (Women and Newborn Service) Perth Children’s Hospital | Geraldton Regional Hospital Hedland Health Campus Karratha Health Campus |
| St John of God Health Care (St John of God Midland Public Hospital) | St John of God Midland Public Hospital St John of God Subiaco Hospital St John of God Murdoch Hospital | |
| WA Country Health Service | Albany Health Campus Broome Regional Hospital Bunbury Hospital Geraldton Regional Hospital |
Each PEHS hosts an information night. You can also choose to work as a rural intern by applying to work through Western Australia Country Health Service.
The intern application process is coordinated by the Postgraduate Medical Council of Western Australia but you apply through the WA Jobs site called MedJobsWA. You submit one application and rank each PEHS from most to least preferred. Selection occurs through panels representing each of the PEHSs. As part of your application, you need to provide a CV (maximum 3 pages) and cover letter (optional) and address the intern selection criteria, you will require a range of other documents as well as nominate 2 referees. If successful you will normally receive a contract for 3 years, which provides you with job security.
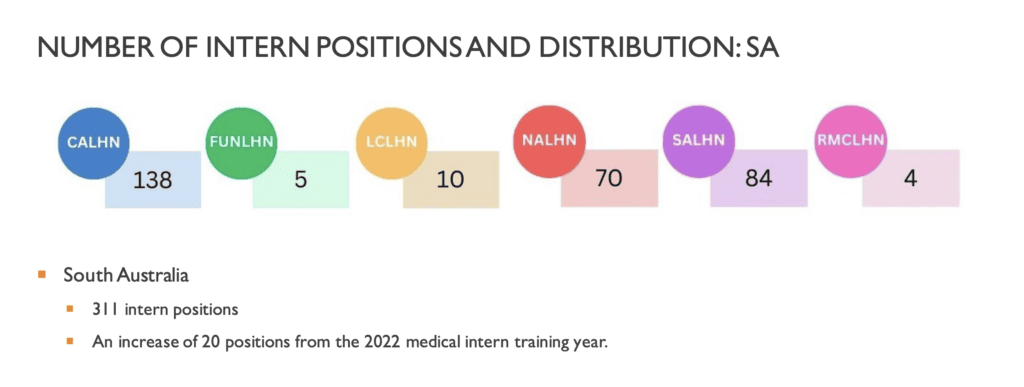
South Australia

Estimated Numbers = 353 (based on 2025 final positions, including 47 rural intern posts)
Annual Salary = $81,814
Length of Contract = 3 years in most cases (IMGs may have shorter contracts tied to their visa status)
Professional Development Allowance = $4,500 per annum
SA MET (South Australia Medical Education and Training) conducts the annual Intern application process in South Australia. There are 3 Adelaide-based Local Health Networks and 3 smaller country-based networks to which you can apply for the priority Rural Intern pathway. It should be noted that whatever network you are allocated to you may request or be required to undertake one or more rotations in other networks.
The Rural Intern Pathway is a strength-based recruitment process for applicants who are interested in undertaking their internship (and potentially subsequent years) in rural hospitals within Country Health SA (CHSA). Rural intern positions provide broad opportunities in unique settings and are best suited for medical graduates with a history of living or working in rural areas or a desire to commence a career in the country.
To apply for internship in South Australia, you must comply with the following criteria:
- Have graduated from a medical school in the last two years (i.e. to start an internship in 2026, you are / were a final year medical student in the 2025 or 2024 cohort).
- Applicants who completed their medical degree at an overseas university NOT accredited by the Australian Medical Council (AMC) must have completed both Part 1 and 2 of the Australian Medical Council exams.
- Can demonstrate that you meet the English Language Skills Registration Standard.
- Be able to commence on the January start date, which includes compulsory orientation, and fulfil the minimum 12-month contract.
- Have completed electronic medical record (Sunrise EMR and PAS) medical student training.
- Be able to demonstrate that you will meet the requirements for registration with Ahpra.
- Have NOT commenced or completed an internship or worked as a doctor before.
- Be an Australian Citizen, Australian Permanent Resident, Australian Temporary Resident, New Zealand Citizen or New Zealand Permanent Resident.
- Have a visa that allows you to work unrestricted in Australia for the duration of your internship.
- Applicants completing their medical degrees in Australia who are on a student visa will need to obtain an appropriate Australian work visa before commencing their intern year (refer to page 33).
- Have completed and submitted an online application, including the provision of valid supporting documentation, by the application closing date.
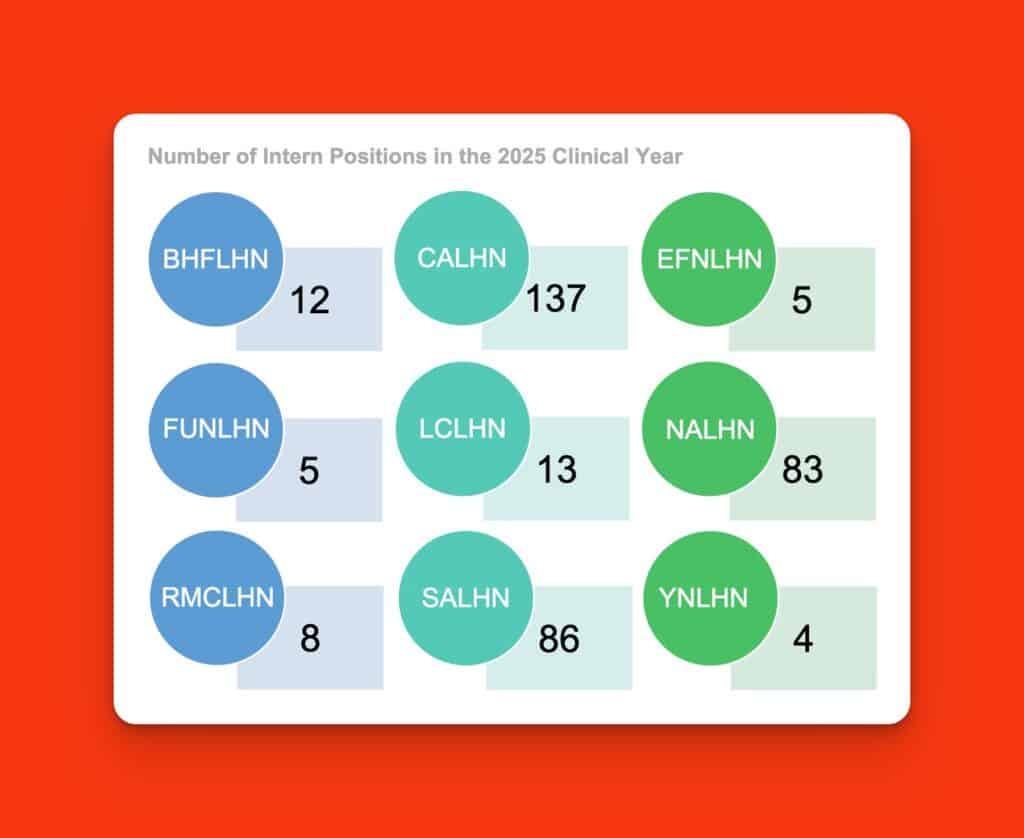
Barossa Hills Fleurieu Local Health Network (BHFLHN)
Central Adelaide Local Health Network (CALHN)
Eyre and Far North Local Health Network (EFNLHN)
Flinders and Upper North Local Health Network (FUNLHN)
Limestone Coast Local Health Network (LCLHN)
Northern Adelaide Local Health Network (NALHN)
Riverland Mallee Coorong Local Health Network (RMCLHN)
Southern Adelaide Local Health Network (SALHN)
Yorke and Northern Local Health Network (YNLHN)
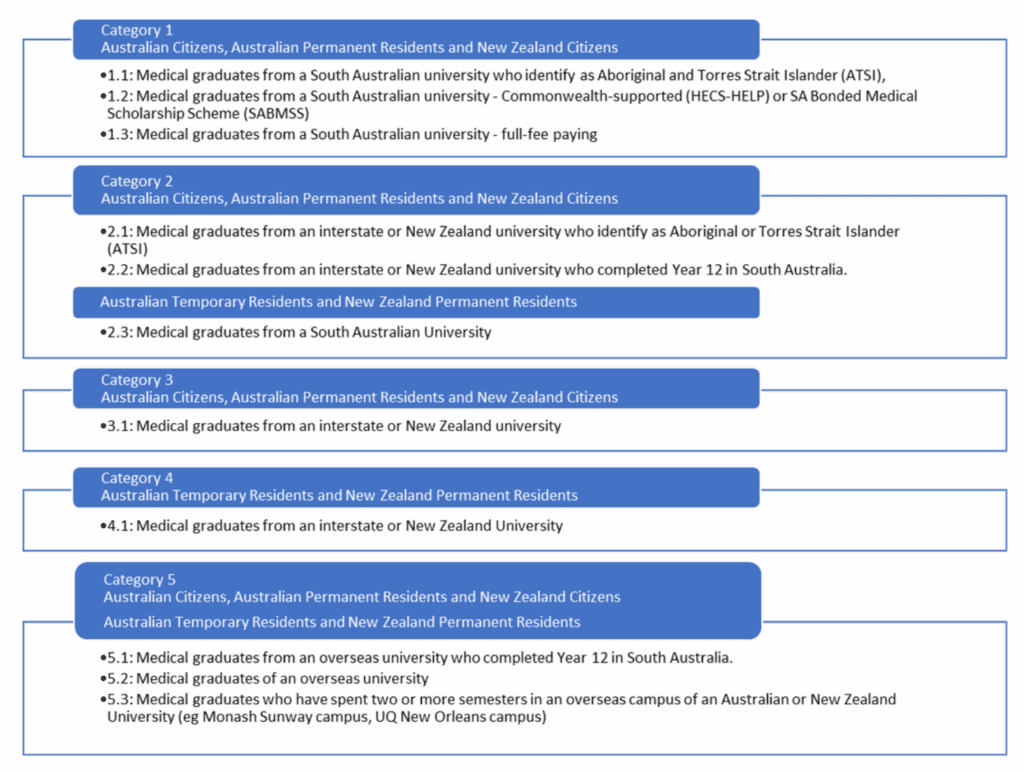
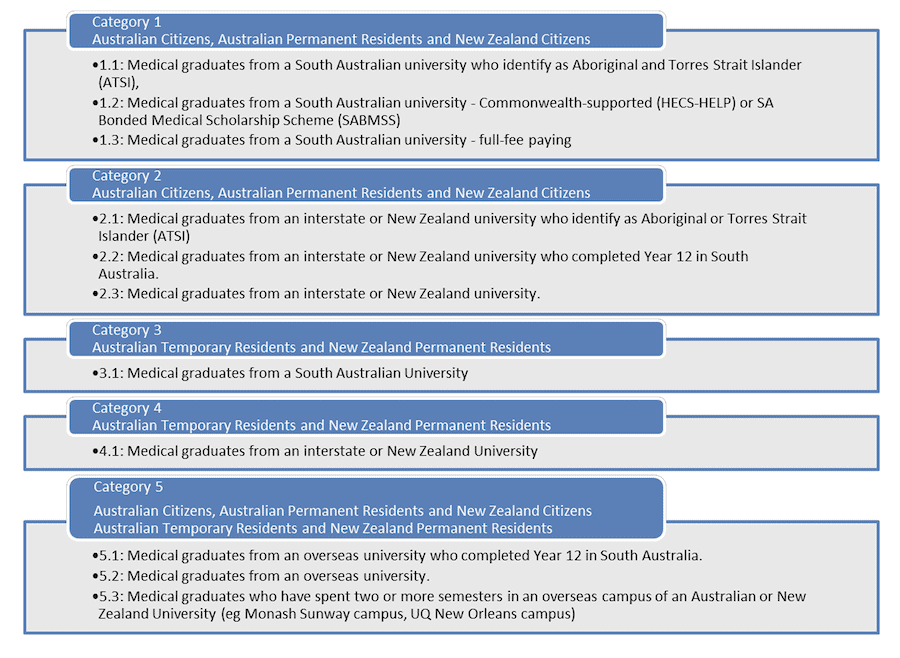
SA Intern Priorities:
Like most other jurisdictions, South Australia prioritises its medical graduates first, then graduates from other States and Territories. International Students are given lower priority than Australian Citizens, Australian Permanent Residents and New Zealand Citizens.
Aboriginal and Torres Strait Islander applicants are given priority preference by being placed in the first subcategory for categories 1 and 2.
International Medical Graduates from non-Australian medical schools can apply for the rural intern pathway so long as they have only graduated in the last 2 years and have completed the AMC Part 1, and can meet the other requirements (which are extensive) and include meeting the Medical Board English language requirements, completing electronic medical record training and have residency status or a visa that allows you to work unrestricted. They must also not have commenced or completed an internship.
International Medical Graduates from non-Australian medical schools can also apply for the main round but in this case must have completed both AMC Part 1 and Part 2.
Rural Intern Pathway
Applications for the Rural Intern Pathway are included in the standard South Australian application for internship.
All applicants are asked to preference all eight rural networks as well as the three metropolitan health networks.
Eligible applicants wishing to apply for the Rural Intern Pathway must preference a rural site as their FIRST preference. Rural Intern Pathway applicants who preference a rural LHN as their first preference are asked additional questions within their application form. And must participate in interviews conducted by a selection panel from the rural LHNs.
SA Health determines which applicants will receive rural internship offers using a preference matching process and the ranked list provided by the LHNs.
The placement of applicants into rural intern positions will occur prior to the placement of applicants into metropolitan intern positions. SA Health will match applicants to specific rural LHNs as instructed.
Internship Categories

Within the respective South Australian category groups, applicants are randomly allocated to their highest possible Local Health Network preference.
If an offer is made, applicants must respond via the electronic application system within the specified timeframe. Where an applicant has been made an offer and no response received, the offer will be automatically declined. Applicants are only eligible to receive one offer for an internship in South Australia.
South Australia is one of few States that specifically permits medical graduates from other countries to apply for internship positions. But they are at the very bottom of the priority list. Please see the above information about the rural internship.
In addition to a CV and referees, in order to apply for an internship in South Australia, you will need to provide a certificate confirming that you have completed the SA Health online electronic medical record (Sunrise EMR & PAS) training.
Tasmania

Estimated Number = 106
Annual Salary = $87,000
Length of Contract = 1 year (attempting to confirm if this has become 2 years)
Professional Development Allowance = nil for Interns but RMOs get an allowance of $2040 per annum
Internships are coordinated in Tasmania via the Department of Health and Human Services.
All applicants are required to apply online. As part of your application, you are asked to preference all of the 3 available sites:
| Site | Number of Positions |
| North (Launceston General Hospital) | 39 |
| South (Royal Hobart Hospital) | 48 |
| North-West (North-West Regional Hospital Burnies and Mersey Community Hospital, Latrobe) | 19 |
Rural Option
You can also preferentially apply for one of 5 places on the Tasmanian Rural Generalist Program. You will be allocated to one of the above sites based on your preference but also undertake a 13-week rural GP placement as part of your internship.
Applying
Applicants must be graduates of or graduating from an Australian Medical Council-accredited University.
All applicants are required to apply online. Only one application is required; you will be asked to indicate your preferred place of employment (Hobart, Launceston, North West Region) via the application form. Applicants must list each site in order of preference.
The online application form ensures all the information required to assess your application is provided. The form includes information on eligibility to work in Australia and details on how to submit electronic reference requests.
The online application form requires you to include your University Student Number and your Australian Health Practitioner Regulation Agency (AHPRA) Intern Placement Number.
Candidates are required to attach a CV/Resume and any other relevant information to their application.
A written statement addressing the selection criteria is NOT required.
Intern Placement Priorities:
The Tasmanian Department of Health currently gives priority, in order, to:
- Australian permanent resident Tasmanian-trained Australian Government supported and full-fee paying medical graduates.
- Australian temporary resident Tasmanian-trained full-fee paying medical graduates.
- Australian permanent resident interstate-trained Australian Government supported and full-fee paying medical graduates.
- Australian temporary resident interstate-trained full-fee paying medical graduates.
- Medical graduates of an Australian Medical Council-accredited overseas University.
Selection
The Tasmanian Department of Health will conduct a ballot-based allocation system for placing Priority 1 (Australian permanent resident Tasmanian-trained Australian Government supported and full-fee paying medical graduates) and Priority 2 (Australian temporary resident Tasmanian-trained full-fee paying medical graduates) applicants.
It is not clear at this stage how further positions are filled according to the remaining priorities.
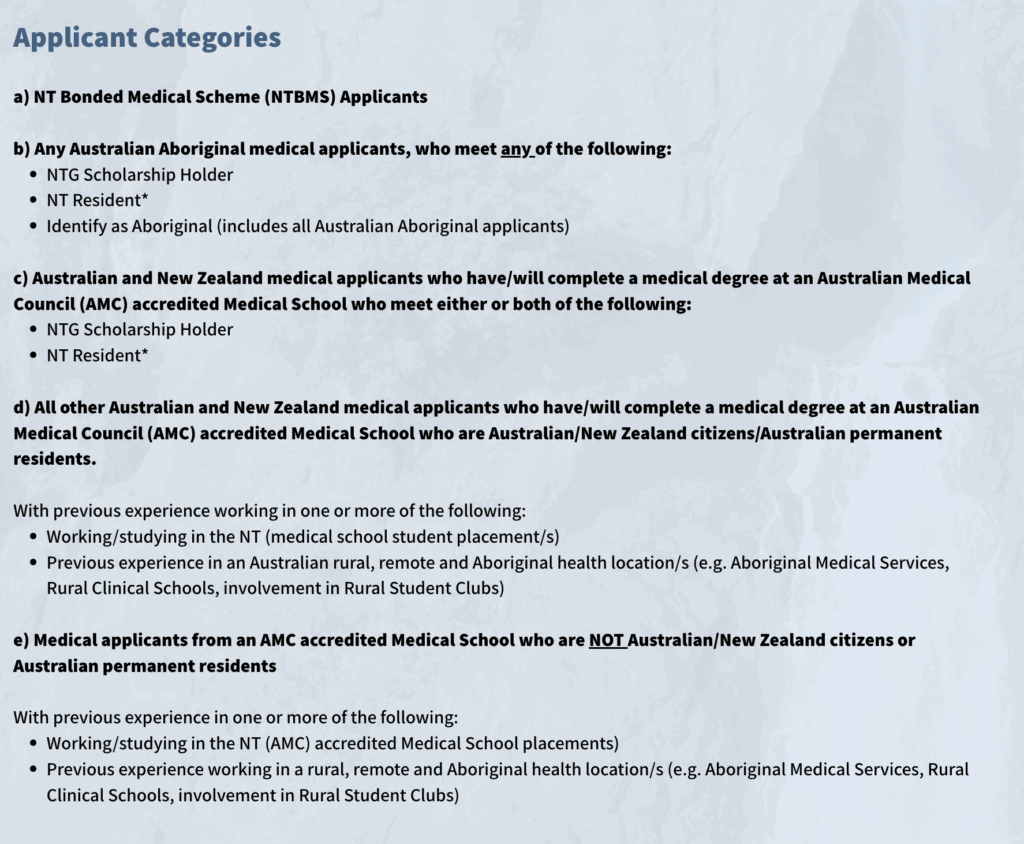
Northern Territory

Intern Numbers = 88
Annual Salary = $90,150
Length of Contract = 1 year
Professional Development Allowance = $3,601 per annum with the option to apply for an additional $3,000 or $3,000 for HELP relief.
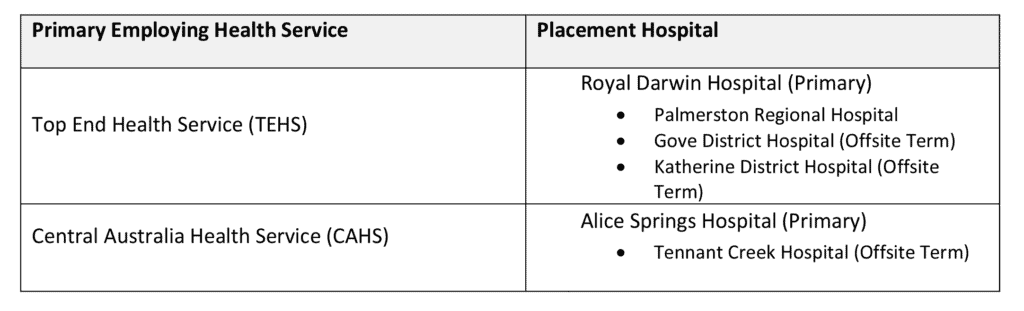
The NT Prevocational Medical Assurance Services (PMAS) conducts a central review of eligible applicants and all intern positions are allocated within the two NT Health Services:
- Top End Health Service (TEHS) – based upon Royal Darwin Hospital (RDH) (64 posts)
- Central Australia Health Service (CAHS) – based upon Alice Springs Hospital (ASH) (24 posts)
Each Health Service has a primary employing health service as well as additional placement hospitals as per below:
Eligible applicants are allocated intern positions in line with the Northern Territory category groups. Within the relevant category groups, applicants are allocated to their highest possible Health Service preference, pending the availability of a position.
Intern Priority Categories:
According to the NTMETC the applicant eligibility categories in order of selection for Internship in the Northern Territory are:
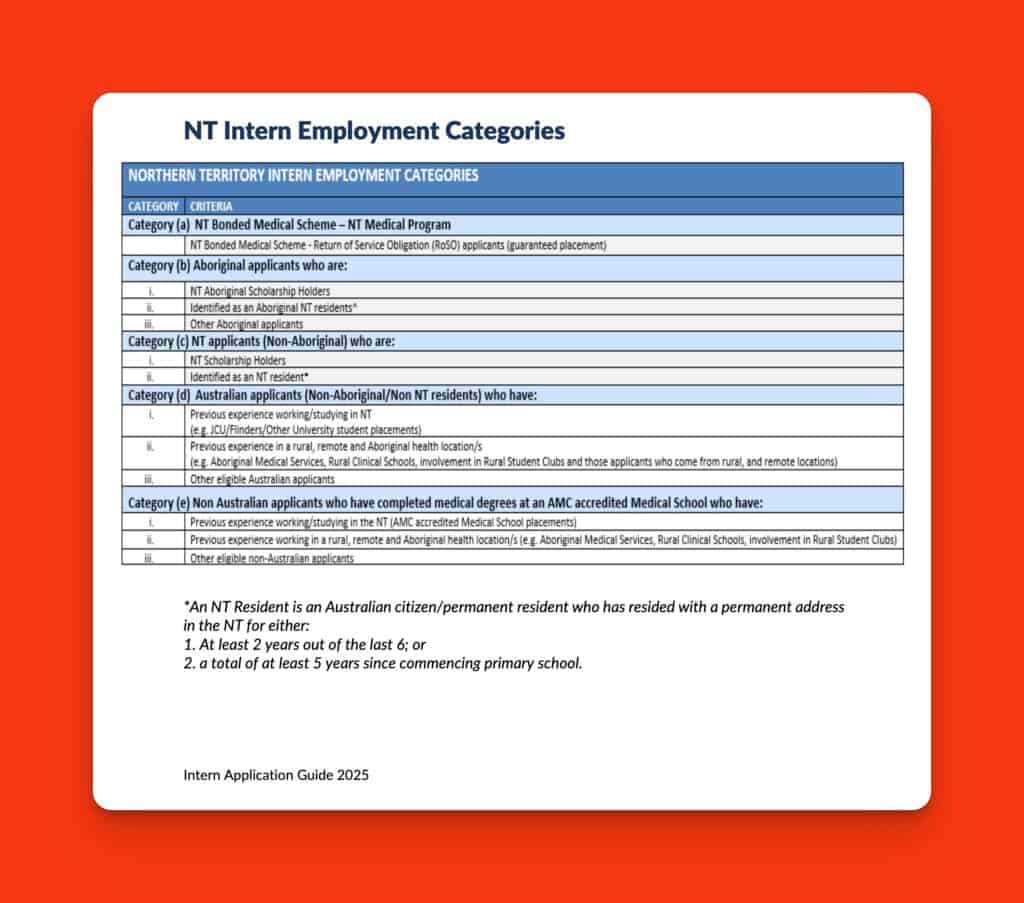
c/- NTMETC
Previously there was an F and G category that provided an option for IMG doctors. It is not clear whether this has been removed for the 2023 year.
As part of your application, you are required to submit a curriculum vitae of no more than 2 A4 pages and address the selection criteria. Applications are submitted to the NT Government employment portal.
Overall the intern allocation process is based on an applicant’s category group, Health Service preference, and the number of positions available in each health service.
The two NT Health Services are responsible for selecting applicants and making their offers of employment, applicants are advised via email. The Health Service responsible for making the offer of employment will after receiving an acceptance from an applicant arrange an employment contract for an Internship position within their health service to be provided prior to commencing their internship.
Australian Capital Territory

Intern Numbers = 96
(6 of these positions are normally guaranteed to NSW medical students)
Annual Salary = $86,619
Length of Contract = 2 years
Professional Development Allowance = $1,150 per annum + $900 Mobile Allowance + $4,000 Relocation Allowance.
If you want to apply for an internship position in the Australian Capital Territory you do so via the ACT Health Recruitment page.
Most of your time is spent at the Canberra Hospital. But ACT is interesting as it is one of the few chances you may have as an Intern to work in 2 separate States and Territories. Rotations may include secondments to Calvary Public Hospital, Goulburn Base Hospital, and South East Regional Hospital (SERH) at Bega. Because the ACT utilises some positions in NSW for intern posts there is a reciprocal arrangement whereby a number of NSW graduates are guaranteed an intern post in the ACT.
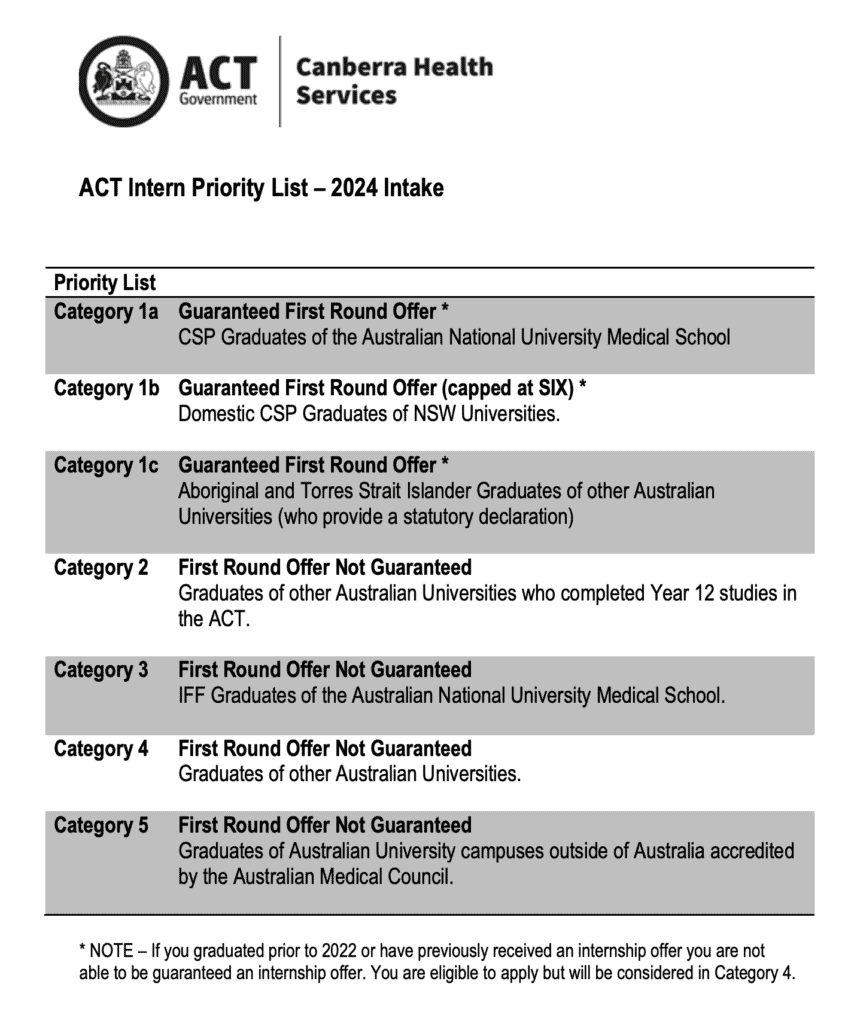
Priority is given to:
– Australian Graduates of ANU
– A maximum of 6 graduates of NSW Universities
– Graduates of other Universities who completed Year 12 in ACT
ACT Intern Priority List:
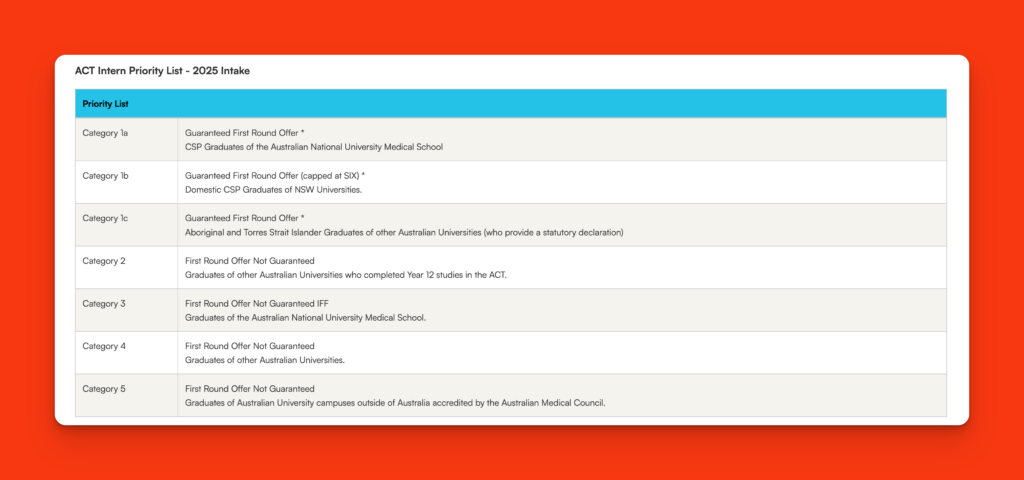
c/- act.gov.au
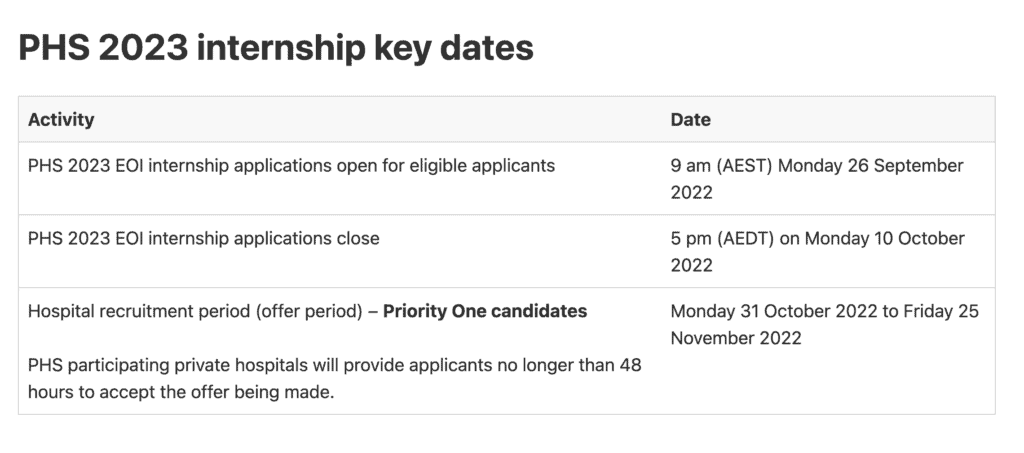
Junior Doctor Training Program (Previously the Commonwealth – Private Hospital Stream)
2025/2026 Information not yet available
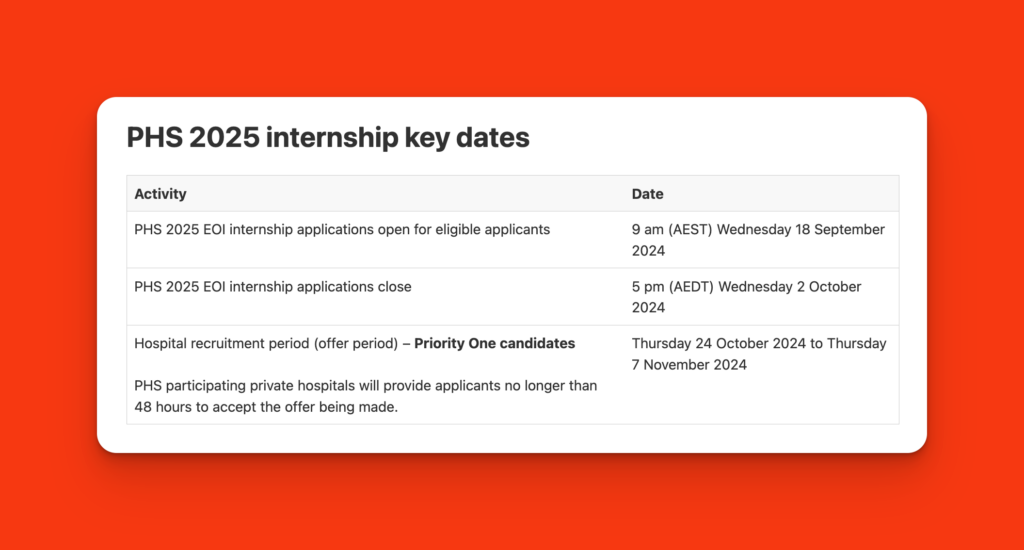
The Private Hospital Stream (PHS) funds private hospitals to deliver medical internships and support junior doctors to work in expanded settings. It focuses on supporting training for junior doctors in rural, regional and remote areas in Modified Monash (MM) 2 to 7 locations.
This includes fostering partnerships between private hospital providers, rural public hospitals and other training settings (such as Aboriginal Medical Services) working as part of expanded training networks.
Annual Salary and conditions should reflect the annual salary for an intern in the State or Territory you are working in.
Internships and places
The PHS supported up to 115 internships and up to 80 PGY 2 and 3 eligible junior doctor places in the 2020, 2021, 2022 and 2023 training years.
Expression of Interest (EOI) internships
An annual EOI internship process is run for junior doctors to express interest in a PHS-funded medical internship place.
This process is only for PGY 1-funded places. It opens each year after state and territory governments have offered and filled their internship positions.
Eligibility
The program divides applicants into 2 categories – Priority One and Priority Two.
Priority One eligibility criteria
The Priority One category is for final year medical students who meet all eligibility criteria for an internship under the PHS.
You are Priority One if you:
- are a full-fee-paying international student completing your medical degree during the current calendar year from a medical school in Australia, having completed all of your medical degree in Australia (university-approved, short-term elective rotations completed overseas are allowed)
- have met the Medical Board of Australia (MBA) English language proficiency requirements for registration purposes
- are not an Australian Citizen
- commit to getting a visa to work in Australia during your internship year.
Priority Two eligibility criteria
You are Priority Two if you:
- have MBA provisional registration as a medical practitioner
- have met the MBA English language proficiency requirements for registration purposes
- commit to getting a visa to work in Australia during your internship year.
Who is not eligible
You are not eligible to apply for the PHS if you:
- do not meet the Priority One or Priority Two eligibility criteria
- have accepted an internship position from a state or territory government.
Recruitment process
The recruitment process aligns with the state and territory government recruitment processes and the national audit process.
Suitable applications are forwarded to the PHS participating private hospitals by the due dates each year.
The PHS participating private hospitals do eligibility checks. They will contact eligible applicants they want to interview.
You should not make direct contact with the hospitals.
Category prioritisation
PHS participating private hospitals must fill PGY 1 places with Priority One applicants first.
If there are still places available after the Priority One list is finished, the hospitals can then recruit Priority Two applicants.
PGY 2 and 3 funded places
PHS-participating private hospitals make their own recruitment and employment arrangements for PGY 2 and 3 junior doctors. This allows them to meet their own service needs.
PHS-funded hospitals
The Commonwealth funded the following private hospitals to deliver the PHS from 2020 to 2025:
- Mater Misericordiae Limited Queensland through
- Mater Health Services North Queensland (delivering PGY 1 places)
- Mercy Health and Aged Care Central Queensland through Mater Private Hospital Bundaberg, Friendly Society Private Hospital Bundaberg, Bundaberg Base Hospital Bundaberg, Mackay Base Hospital Mackay and Mater Misericordiae Hospital Mackay (delivering PGY 1, 2 and 3 places)
- Greenslopes Private Hospital, Queensland (delivering PGY 1, 2 and 3 places)
- Calvary Health Care Riverina, New South Wales (delivering PGY 2 places)
- Mater Hospital Sydney (delivering PGY 1 places)
- St Vincent’s Private Hospital Sydney (delivering PGY 1 places)
- MQ Health, New South Wales (Macquarie University Hospital) (deliver PGY 1 places)
- St John of God Ballarat Hospital, Victoria – Grampians Intern Training Program (delivering PGY 1 places)
- Ramsay Health Care, Western Australia (Joondalup) (delivering PGY 1, 2 and 3 places).
How To Decide Where to Apply for Your Internship?
There are lots of considerations when it comes to putting in your Intern application. Everyone is a bit different. Some graduates feel like they would like to be close to home and family whilst going through their transition to Intern. Others see it as a chance to get away and explore a new place and location. And then others focus on the long-term career prospects of certain locations.
I think this last consideration is a little overrated for most. You can generally experience a wide range of medicine in your first couple of years of medicine after graduation and there is scant evidence that this affects your prospects of applying for specialty training posts.
That being said if you have an interest in anything other than Medicine, Surgery or Emergency Medicine as a future career you should probably investigate whether this particular specialty is offered at the hospitals or networks to which you apply.
Unfortunately, the internship model in Australia is quite antiquated and we have continued to use the experience as a proxy for competency when a large portion of the medical education world has moved on. The result has been the mandating of the 3 core terms for the internship of Medicine, Surgery, and Emergency Medicine. There is really no solid educational basis for this approach and one of the unfortunate outcomes is that all the other specialties get squeezed out and few interns get to experience psychiatry, general practice, obstetrics, paediatrics, pathology etc… which ultimately does have an effect on recruitment to these specialties.
So the basic message is this. If you are really dead set keen on doing radiology as a career you should try to track down the very few locations that might offer this rotation to either interns or residents.
Each year the Australian Medical Students’ Association produces a very useful Intern Guide with lots of information about the composition of intern training networks across the country. The 2023 version is not available but here’s a link to the 2022 version.
Frequently Asked Questions
Is There Any Restriction On Where I Can Complete My Internship?
Can I Apply to More Than One State or Territory for an Intern Position?
What is an Intern Placement Number?
I Am Not an Australian Medical Student. How Do I Obtain an Intern Placement Number?
What If I Have Special Circumstances Which Make It Hard For Me To Work In Certain Places?
I Have Received My Intern Offer. But I Would Like to Defer It. Is This Possible?
I am a Doctor With a Medical Degree From Outside Of Australia. Can I Apply For an Internship?
I Have Heard That Some Graduates Miss Out On Internships. Is This True?
Can I Submit a Late Application?
When Will Offers Be Made in 2025?
What if I Receive More Than One Offer?
What is the National Audit?
What if I Don’t Respond to the National Audit Data Manager?
What is the Late Vacancy Management Process?
Who can participate in the Late Vacancy Management Process?
Can International Medical Graduates Apply to Become an Intern in Australia?
Can International Students Apply to Become an Intern in Australia?
Can I Swap Intern Posts?
Can I Defer my Intern Offer?
Can I Be Allocated to the Same Spot as My Partner?
Can I Do My Intern Part Time or Job Share?
What If I Have Special Circumstances?
(Disclaimer: All information here has been sourced in good faith but things do change so you should always do your own due diligence in such matters, we are providing this information to aid you in your application but take no responsibility for any outcomes)We’d welcome feedback from any Intern programs in relation to the accuracy of the above information.