This is an evolving blog and vlog post specifically about how to write a medical student resume put together by request from a number of medical students who have contacted me asking for this type of information.
In my experience, many medical students are at a bit of a loss composing a resume in their final years of medical school. There may be a number of reasons for this but high amongst these reasons is the fact that for many it’s their first experience at doing something like this. So before I dive into the details and specifics lets me give you my key tips on how you can get a good medical student resume together.
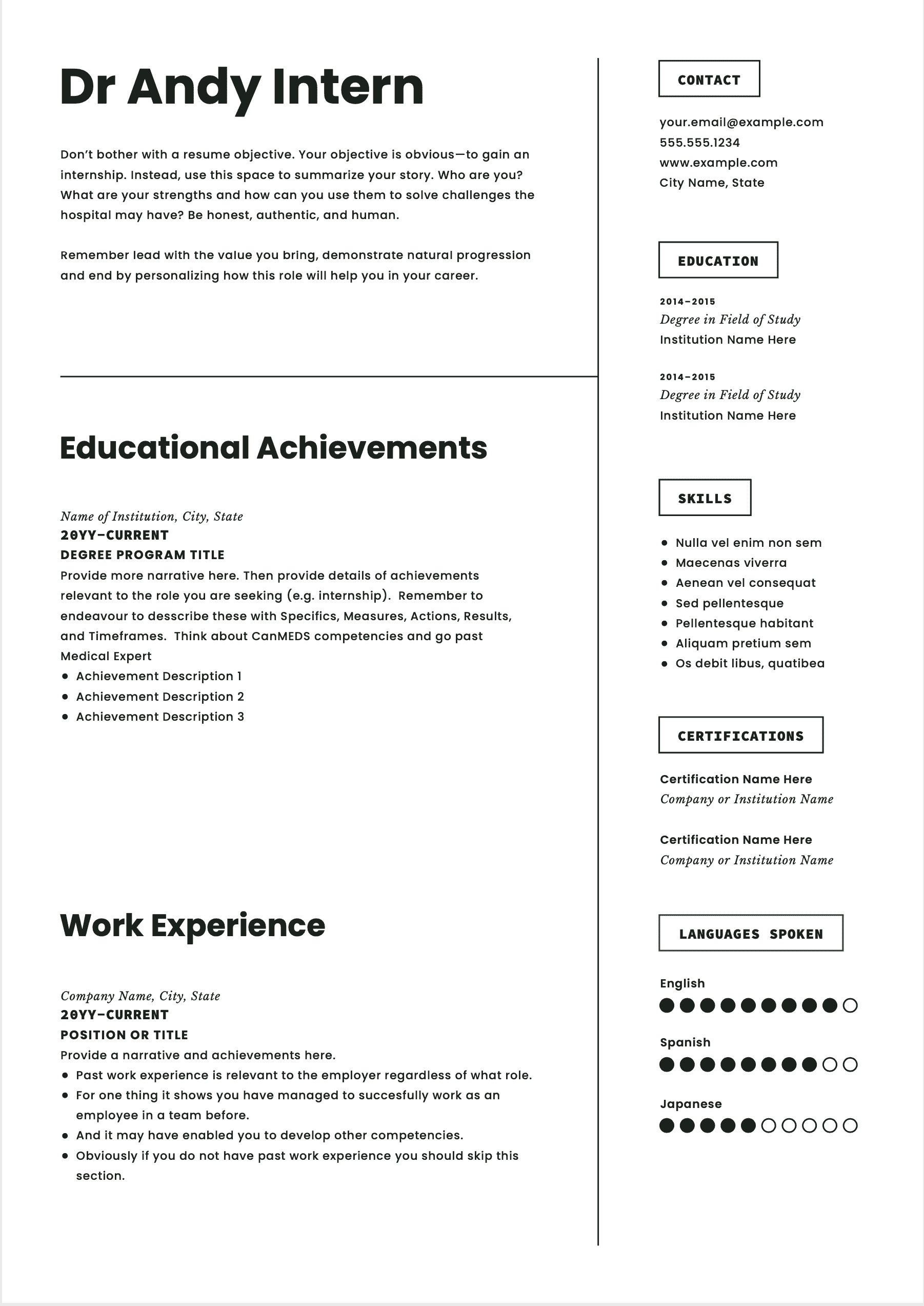
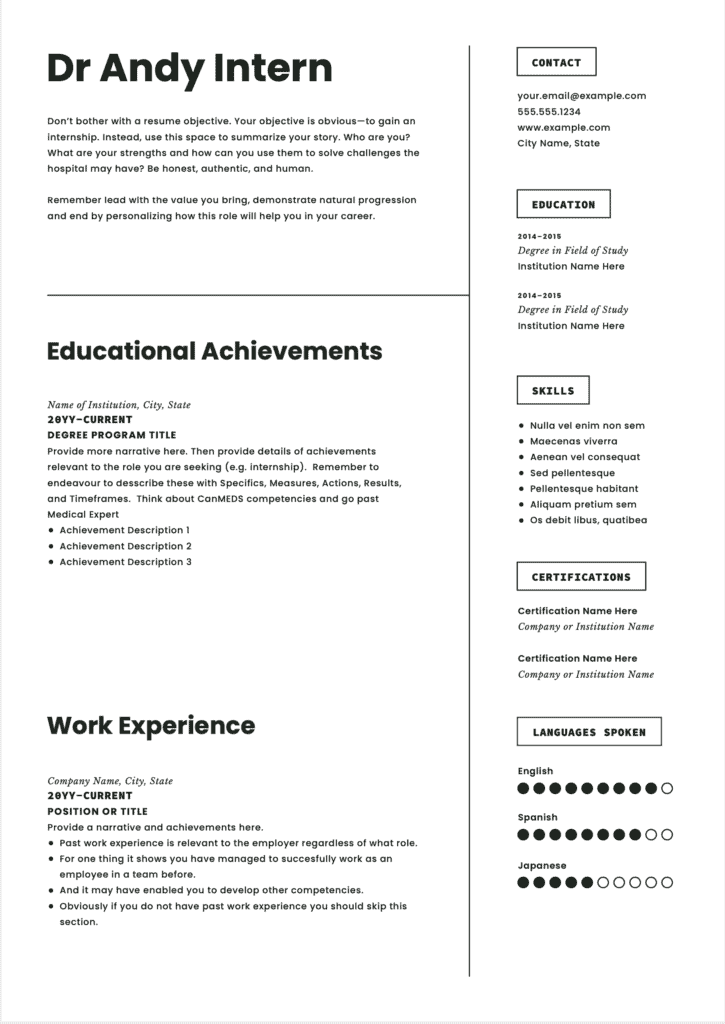
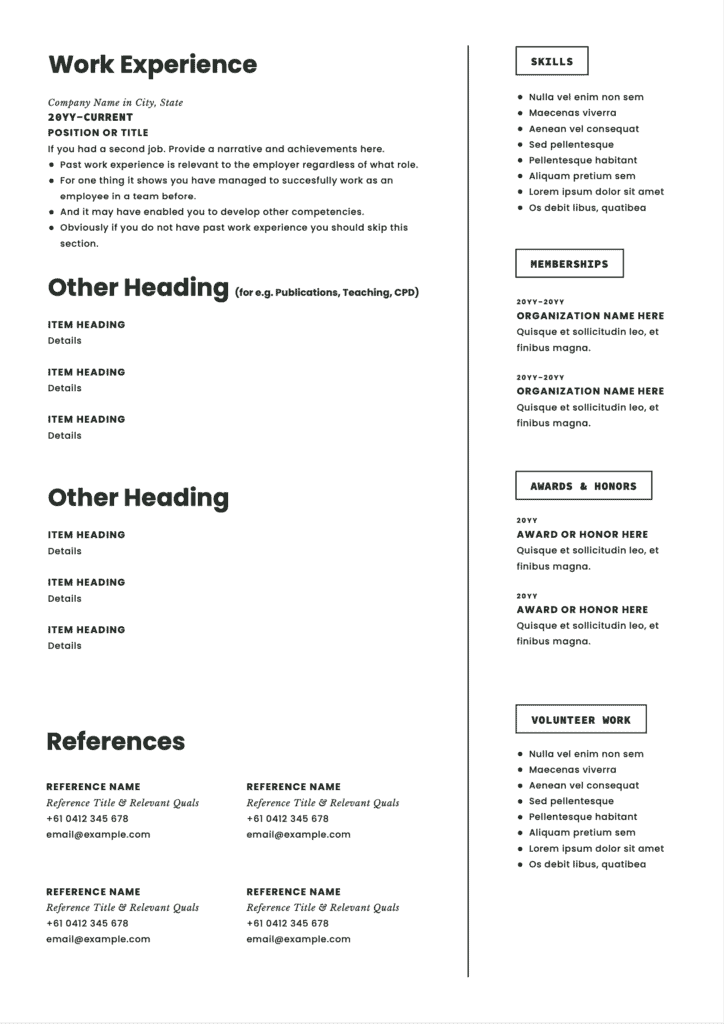
- It’s really helpful to start with a template. Problem is there are not too many that are specifically for medical students. So I’ve supplied you one at the end of this post (to encourage you to read the whole way through).
- It’s best to not get caught up with particular headings or what should go where. Just start writing in the sections that you can and get the juices flowing. Leave your personal statement to the very last.
- Understand that employers spend only a few seconds the first time they see your resume. So in order to maximise its impact, you need to ensure that important matters are on the first page.
- Personal statements can be tricky to construct. Especially the first time you try to do it. For most of us, it’s hard to talk ourselves up. In this article, I have provided a personal statement formula that works well for most doctor’s
So, if you are a medical student and would like some help with your resume you are in the right place. And look even if you are not a student you may find some of these tips useful so please feel free to keep reading as we dig a bit deeper.
What Is Unique About the Medical Student Resume?
There are a number of unique features of the medical student resume. And I should clarify we are talking here about the one that you put together at the end of your medical school years. The one you need for your intern application.
A key unique feature of the medical student resume is that it can be a struggle to show big points of difference at this point. You might be lucky to have won some awards or have a higher than normal grade point average in your medical school. But generally, most medical students have the same types of experiences and learn the same things in medical school. So, this can make it really hard to stand out.
On the positive side, there is generally less emphasis on the importance of your resume at this point. The key reason for this is that from an employer perspective you have not been tested as yet through work experience. Work experience is a key thing that most employers look at on any candidate’s resume.
So with a similar educational experience and lack of any work experience (at least as a doctor), it can seem hard to stand out.
Or can it?
Describing Competencies Can Boost Your Resume.
I recently gave a seminar to some 4th-year medical students (students in their penultimate year) at my local university. The talk was about the importance of being well-rounded in one’s medical career and being able to demonstrate a range of competencies on your resume.
Being able to articulate your competencies and demonstrate evidence for them is a really good way to shine on your resume. The problem is many medical students and doctors alike don’t know what competency is. Which is a real shame as competencies underpin much of what is currently occurring in medical training.
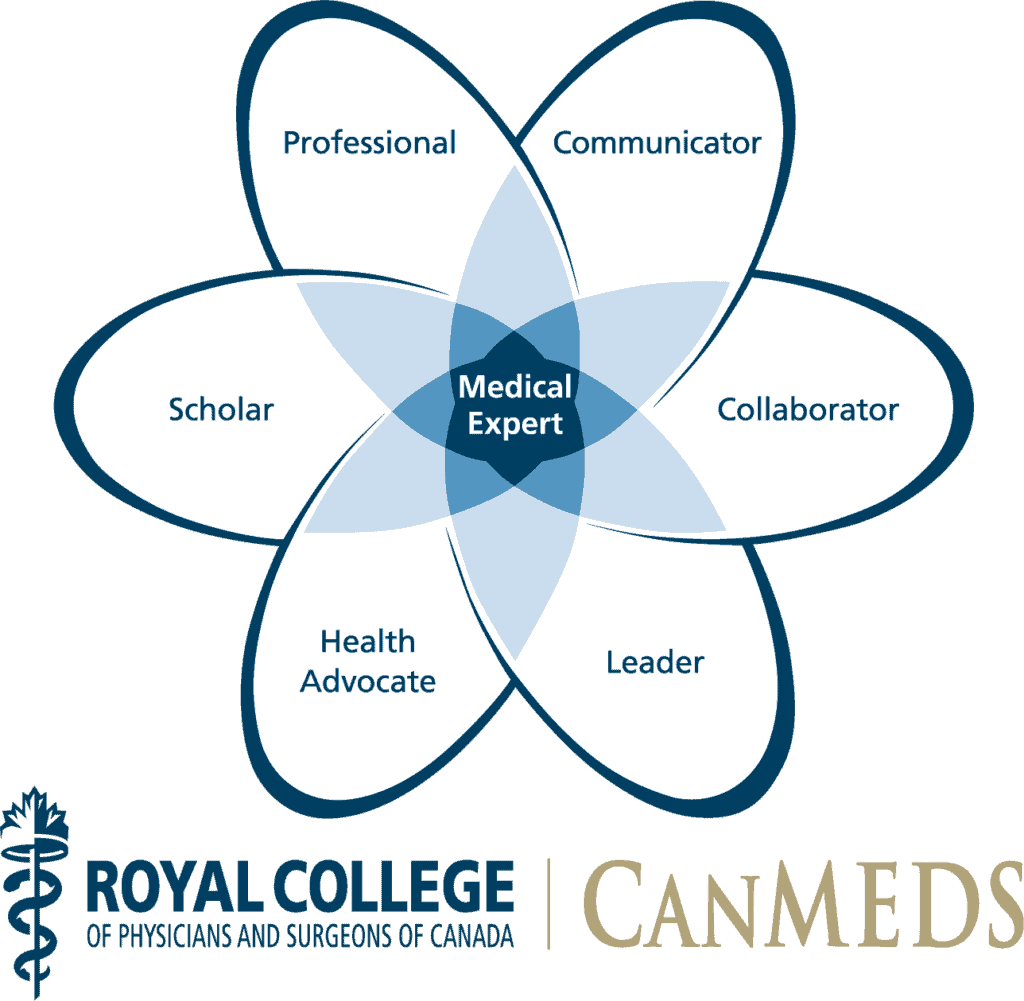
The framework I like for describing competencies is the CanMEDS framework. I’ve done a few more extended videos about CanMEDS so here’s one of those videos if you want some further details.
But suffice enough to say, CanMEDS is a thoroughly well-tested model that says that what we are looking for in a good doctor is someone who is not only a medical expert but has strengths in the areas of communication, collaboration, advocating for patients and good health outcomes, scholarship (i.e. teaching, learning and research), being a leader and of course being a professional.
All good so far when I
spoke to my students about this concept.
They could all see that there was more to being a doctor than their
medical knowledge and skills.
BUT they asked
me. How can we actually demonstrate that
we have competencies in those areas?
What are the
opportunities we have between now and graduation where we can develop these
other competencies more or demonstrate our proficiency?
Fair enough question.
So let’s take one of these competencies. Let’s take communication.
I have deliberately chosen communication as it can be an extremely difficult competency to write about in a resume. Yet it’s almost always there as a key selection criterion.
Lots of doctors (not just medical students) will just write that they are very effective communicators.
I am a highly effective communicator
Typical statement seen on a doctor resume which frankly means nothing.
But so what. Who says? Where’s the evidence?
Well. If you think about it for a minute. In medical school, there are actually plenty of opportunities to demonstrate your capability as a communicator and collect evidence for your resume.
You just have to be
strategic and have a bit of a plan.
If you just rely on what the medical school says to guide your learning you are going to miss these opportunities that I am now going to point out for you.
Communication Opportunity Number 1.
Communication Training sessions.
Most medical schools these days incorporate specific sessions or training around communication. Engage in these sessions. Find out what the curriculum or learning outcomes are for them. Write these learning outcomes down in a logbook or a diary somewhere.
Go into these sessions with a specific goal in mind. If, for example, you feel that you want to work on counseling patients, as part of your communication training. Tell the teacher of the workshop this at the start and ask if there is a specific opportunity in the session for you to practice this aspect of your communication.
Write a short reflective piece about what you learned as a reminder and reinforcer.
Now. When it comes to
putting your resume together you suddenly have something substantial to write.
For example,
as a communicator, I was trained and assessed in my medical school training to be an effective and patient-centred listener and communicator. I learnt the benefits and utility of various communication techniques, including both open and closed questions. I learnt how to successfully handle difficult communication challenges, such as breaking bad news or enquiring about suicide. A personal goal for me in all of this was to achieve high-quality counselling skills, which I am pleased to say I was able to achieve so that I am competent in a range of counselling situations for interns, including discharge planning, the impact of lifestyle on health, and discussing common medications and their possible side effects.
Communication Opportunity Number 2.
End of Term Reports.
Most medical schools will require that you get some sort of end-of rotation or end-of-term supervisor report. Use these to collect feedback and information about your communication strengths and weak points.
I would encourage all
medical students to start out each rotation again with a few clear learning
goals in mind. If communication is one
of these. Make sure that this is clear
to the consultant and the trainee doctors and other team members that you are
working with.
Be as specific as
possible about what it is that you are wanting to work on. And encourage them to be as specific as
possible.
So again, going back to our previous example. Perhaps you want feedback on your counseling skills. Say this upfront and your team will most likely help construct opportunities to practise these skills and get feedback.
At the end of this rotation and others. You will then hopefully have meaningful comments in your supervisor reports which you can use on your resume. Check with your supervisor about your end-of-term reports before the term wraps up. Make sure that you are provided with plenty of written feedback.
Then when it comes to
putting together your resume. You have
more to write about.
For example,
across my last 2 clinical years of medical school, my supervisor reports consistently showed that I excelled in communication. I was signed off as competent in being able to gather a relevant history, make appropriate file notes, complete an effective discharge summary, conduct a handover and do basic patient counselling.
Communication Opportunity Number 3.
So, my final
opportunity for you to both enhance your communication and demonstrate it on
your resume might be seen as a little bit more unorthodox than the last 2
suggestions.
But I’d encourage you
to consider this one.
As someone who has
interviewed thousands of doctors over time for various jobs. There are few things that speak more highly
about someone’s communication skills than actual patient feedback.
Very few doctors
bother to gather feedback from patients about things like communication.
So here is a really
great opportunity for you to stand out.
Think about putting
together a short survey or questionnaire for the patients you are seeing. Make sure of course that you consider issues
of consent and privacy. It’s probably best not to collect any demographics or
even case details.
Whenever you see a
patient ask them if they would mind filling out a quick survey about your
communication.
Very quickly you will
be able to compile a useful set of data and information that will probably show
you your areas of strength (which you can now point out on your resume) and
areas for improvement.
For example,
During medical school I also conducted a survey of 20 patients who indicated that I was an effective listener, was able to communicate in lay language and that they would be more than happy with having me as their intern.
So there you go.
Some tips about how to
talk about your communication on your CV.
Some of these you may be able to act based on existing data that you
have collected. Some may require you to
think about the remainder of your medical student days.
Personal Statements
One of the most crucial elements of any resume is your personal statement or what is sometimes referred to as your career goal statement.
If you don’t know what a personal statement is. It’s that piece of narrative text that normally immediately follows your name and brief details on your resume and summarizes you as a job applicant.
Other names for personal statements are:
- Personal summary
- Personal profile, and
- Career goal statement
Now. If you have watched any of my videos about CVs and resumes you will know how important I view your personal statement to be. It’s possibly the most important part of your resume.
And personal statements are even more important. If that’s possible. When it comes to medical student resumes.
This is because you have no formal on-the-job experience as a doctor. Which is normally the next most critical part of your resume.
Benefits of Personal Statements on Medical Student Resumes.
So, let’s talk first briefly about the benefits of a personal statement and we will go over how you should construct your personal statement.
The benefits of a personal statement really boil down to one big thing, which is your ability to control the narrative of your resume.
Think about it. If a prospective employer has not met you before. And they are reviewing your resume along with a bunch of others. Having a quick snappy well-written summary at the top of your resume is like gold to them.
It saves them time by giving them key things that they need to know.
Think of it as the abstract on a research paper or an executive summary on a report. How many times have you read one or other of these and then not even bothered reading the rest of the paper or report? Or possibly just skimmed the rest. I’m betting it’s at least 9 times out of 10.
People only have limited memories and like it or not they are going to try to simplify you. To make it easier on them. So what is better than to control this simplification through the use of a well-constructed and controlled statement on the top of your resume?
Why not control the narrative of your career rather than them making it up by hopping all over your CV?
And even if they do know you. Which happens a lot in medicine. The summary is still going to help them in that simplification. As they really know everything about you.
So that’s why a personal statement is crucial.
Let’s now talk about how to construct one.
How to Construct a Personal Statement for Your Medical Student Resume.
So, in order to construct your personal statement, you are going to need a few other things as well.
First. You should ideally have written at least the first draft of your resume already. You need that. Because personal statements should link to the other components of your resume.
Secondly. You should also ideally have a position description. Now, this may be hard depending on where you are located. If you are in Australia or New Zealand you are normally applying for an intern position at a number of locations across these two countries so there may not be a clear job description. In the UK it may be a similar issue applying for foundation posts. For residency applications in North America, there may be a job description available for the post.
Normally there is some form of document that has the selection criteria on it. Which is what we are looking for.
What we are endeavouring to do is match our best strengths to the job and tailor our resume and statement as much as possible.
So, once you know what the key things the employer is looking for. Think about the key strengths or key skills that you have in your resume which match these criteria.
We have already talked about one of these in our previous topic about talking about communication in your resume.
Communication almost always comes up as a key selection criterion for intern and resident posts. It’s so crucial that you have good communication skills.
A Formula for Great Personal Statements.
My formula for personal statements is as follows:
First off start by telling them what you can offer them. What value you do you bring. It’s really important that you lead with this first. Employers are looking for people who can add value to their organisation even if it is future potential. You are being respectful by offering something first.
So for example as a medical student you might say something like:
I have recently graduated from one of Australia’s most innovative medical school training programs where I developed strong clinical capabilities along with excellent communication and teamwork skills as evidenced by high ratings in communications workshops and excellent supervisor reports which I have listed in my resume.
It’s important that you provide some measure justification for your strengths even if it is referring to someone independent, particularly with something like communication.
The second part is that you need to show them why this position is a natural next step or fit for you. Now, this is relatively easy to do for a medical student resume. But there is an opportunity to personalise things a bit.
For example,
In seeking this internship opportunity, I would strongly welcome the opportunity to work in your hospital as I feel that I have already developed a strong understanding of the organisation through my 12 months on placement.
Finally, you want to leave them with a personal reason for why you feel you are a good fit for this particular job. Now, this may be a little bit hard if your resume has to be submitted to a number of hospitals at the same time. So, it might be a little difficult to personalise it down to that level. But if you can then do so.
One way of achieving this is to make your personal statement a career goal statement.
Converting from Personal Statement to Career Goal Statement.
So, we can do this by finishing off our personal statement by talking about where we see this job helping us or taking us into the future (let’s say in about 3 to 5 years time).
For example
Working at this hospital will, in particular, give me a strong opportunity to develop my passion for general medicine as it is one of the few tertiary facilities in the State that has retained a general medicine department. Ultimately, I would love to do my basic physician training at your institution.
If you can point out something that’s good about the hospital and make reference to seeing yourself working there for a good while then employers love that.
So that’s one example of a medical student resume personal statement.
Because it can be hard to craft one of these the first time. Let me leave you with a couple of more examples.
Example of A Personal Statement for a Doctor Targetting a Rural Internship.
I offer a commitment to rural medicine.
Example of a Personal Statement for a Medical Graduate Targetting a Hospital With a Particular Program.
Referees.
Now that you’re entering the final years of medical school, it’s time to start preparing for your transition to becoming a “real doctor”. In Australia, we call this the internship. But you might refer to it as other things like your residency or foundation program. Depending on where you are in the world.
Now the requirements for applying for an intern post vary a little bit depending on where you are applying.
But one thing that most of you will need to consider is having referees for your application.
So in this section, I’m going to talk about.
- How to go about finding referees.
- What sort of referees you should consider.
- And of course how to list your referees on your resume.
References are required for intern applications in most States and territories of Australia. But they’re not required in New South Wales if you’re going through the general application system. But if you are applying for the rural preferential system, they are required.
So basically, most Australian medical students need referees.
What exactly is a referee?
Basically. A referee is someone who agrees to have their name and contact details listed on your application and resume so that the selection panel can contact them to ask questions about you.
These questions might just to confirm that you are who you say you are. Or may go quite a bit deeper seeking to validate things you say about yourself on your application and get a better feel for how you operate from another person’s perspective.
So, it’s pretty important to choose your referees wisely. More about this soon.
Now the first thing you should be thinking about before you get to selecting referees is to be thinking where you might be applying for with your internship and checking out all the requirements that there are including what sort of documents you may need to submit.
In general, you will need to submit the names of at least two people who can vouch for the fact that you’ve been a medical student and preferably talk more about you than that.
It’s generally wise also to have a third referee just in case.
In most cases, it’s ok for your referees to be supervisors that you’ve worked with, a faculty member or even something like a professional staff member. It’s best to have at least one medical professional as a referee.
In a few cases, there may be requirements are for all of your referees to be medical professionals, particularly in certain other countries. So again, you need to check out the actual requirements.
How to Approach Potential Referees As A Medical Student.
So here’s my suggestion for how you should go about collecting referees.
After you’ve completed a placement or rotation, you should consider approaching your supervisor to ask if they would be happy to act as a referee for you.
Explain to them carefully that you don’t need them to do anything at this point.
It may even be that they just need to be listed as a name on your application. Just write down their contact details including:
- The correct spelling of their name
- Their title or position in the hospital or facility
- Their best email and phone number
Is preferable to get a mobile or cell number, if they’re happy to give this. Tell your referee that you may need to contact them in a few month’s time to act as a referee. Make sure they don’t get too carried away now and start writing you a letter of reference (unless you truly think that you may use this).
In my experience, in most cases, referees for internship posts are not actually contacted or just quickly contacted to verify you are who you say you are.
Now. Before you end this rotation. Think about the other members of the team. Who did you get on well with? Who did you respect? Could they also be a good potential referee?
Think about specialty trainee doctors, Nurse Managers and Allied Health staff.
Repeat the step you just went through with your supervisor to ask these people for a reference.
Pretty soon in a very little amount of time, you will have a bunch of options for referees for your resume and application.
Does Brand Recognition Matter for Medical Student Referees?
Now. Some people say it’s a good idea to collect the names of well-known people as your referee. You might call this going for “brand recognition” on your resume.
In my experience, particularly for the internship applications, it makes little difference whether you have a well-known person on your resume.
What is more important are a few other matters.
Recency, Relevancy and Diversity Matter More for References on Medical Student Resumes.
When selecting your referees it’s a good idea to think about 3 key points
- Recency
- Relevancy
- Diversity
Let’s unpack that a bit more.
Recency
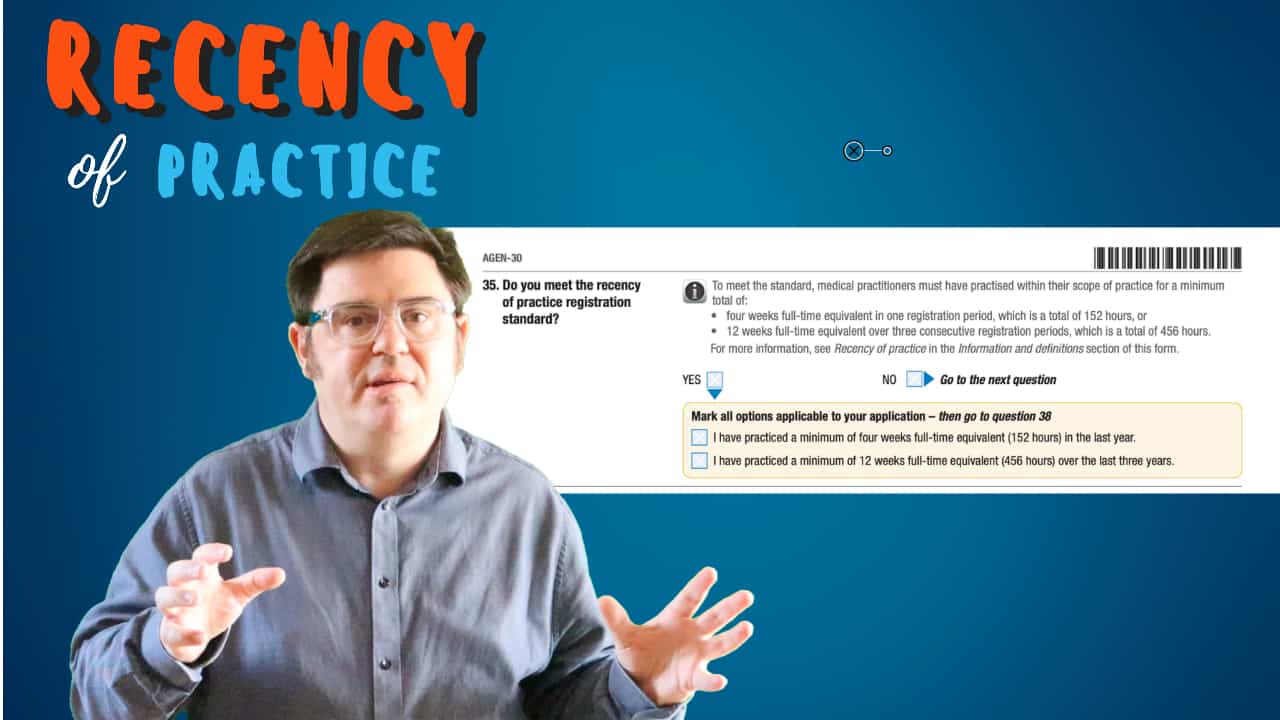
Recency is about having referees with up to date knowledge of your performance. As a medical student, you probably have a number of options here. Try to ensure that your referees have had some contact with you in the last couple of years. And in particular, make sure that one has had a good view of your performance in the last 12 months.
Relevancy
Relevancy is about someone speaking to the role that you are going into. Amongst your referees, you ideally need one or two who have an idea about the job you are going to perform. Clearly, for a prospective intern, this means having at least one medical referee. But think about this more deeply. Are you perhaps applying for a rural internship? If so, it really makes sense to have at least one rural doctor as a referee who can attest to your aptitude for rural medicine.
Diversity
Diversity. is probably the most often overlooked of the criteria. You don’t need to have all doctors on your resume. And these doctors don’t need to be all-male consultants over 50. A good way to show that you can work well in a diverse health team is to have a range of referees on your resume. At least one male and female is a good start. But think also about registrars, as well as nursing staff, allied health and managers. Often these people get a much better look at you than a consultant. So make a more effective referee anyway.
How to Know If A Referee Will Be a Good Referee.
I am often asked how to tell whether a certain referee will be a good referee. The best way to assess whether someone will act as a good referee for you is the direct approach. Ask them.
Ask them what they would say about you if approached for a reference. Most people will be honest with you. If someone feels like that they can’t give you a great reference they will probably say so. And you will likely learn something vital about yourself in doing so.
It’s worth noting, however, that you probably don’t want someone as a referee who tends to be really overenthusiastic about your performance (to the point where you don’t feel you merit at all their praise). This may come across as lacking in authenticity when they are rung up.
From a recent literature review, I was involved in there was some small (limited) evidence that choosing a more junior or younger referee may provide a more positive reference. But honestly, I wouldn’t make this the key criteria for choosing your referee. Because as I say the evidence was small in its significance at best.
Finally, you are probably wondering how to go about listing your referee on your resume.
How to List Your Referees On Your Medical Student Resume
Example of how to list your referees
Basic Physician Trainee example:
Dr Michael Reeves (FRACP) Cardiologist and current supervisor, Regional Hospital, Regional City 0444 555 666 777, email@advancemed.com.au
Of note, you want the name, their title, where they work and a mobile number and email address for contact. You don’t need to include all of their qualifications. But anything that relates to your job application (in this case we are wanting to become a Fellow of the RACP) can go in. If it is unclear from your work history how this person knows you make sure this is explained as well.
So remember:
- Recency
- Relevancy
- Diversity
Describing Your Education and Other Achievements
One thing that is unique about a medical student resume over other doctors resumes is the absence of work history. Or at least the absence of medical work history. It’s one of the rare situations where it generally makes sense to put education next after your personal statement.
But don’t forget to include any substantial work history. That job you did in a previous life as a management consultant for Deloitte’s might just be the big thing that stands you out over other candidates.
In terms of describing your education history. Much the same as for your work history. You should see this as an opportunity to highlight your ability to perform and achieve.
Don’t just put down a list of your medical curriculum requirements. This is boring and the employer will just assume that you did the same thing as everyone else at your school.
Try to find opportunities to show that you can stand out and did more.
For example, was there a particular clinical rotation where you were given some additional responsibility? Or perhaps took on a small audit for the unit. Or did you take on a leadership role in your medical society and did you actually achieve something in that role?
Be SMARTE
Use the acronym SMARTE to describe your achievements.
SMARTE stands for
- Specific task or Situation: describe the actual task including specific details. Create a “mental picture” of the accomplishment.
- Measurable details and Metrics: quantify the accomplishment use facts, figures, dates, and percentages.
- Actions taken and your Actual role: talk about your actual involvement in the change, were you in charge? did you take on a key role? did you show initiative? Acknowledge team contributions wherever possible (Medicine is a team game) but make it clear that you made an active contribution to the teams’ success.
- Results achieved and deliverables defined: describe the overall outcome or final product, it’s overall quality compared to some important benchmark, inform the reader if you received any positive recognition for the work.
- Timeframe to accomplish the task and the Team involved: talk about the time to create the outcome and the other members of the team. Especially if you met your objectives in a period of time that was under pressure (where it often was) or earlier than expected. And if you displayed good teamwork skills in getting other members on board.
- Environment, culture and underlying circumstances: talk about the challenges that may have been present in the environment and how you overcome barriers.
Now not every achievement will have all of SMARTE in it. But the more the better.
Here is an examples
During my Cardiology term as a final year medical student, I was placed on one of the State’s busiest units. On a weekly basis I was regularly helping the intern to clerk 24 inpatients along with attending the weekly general outpatient clinic, 2 stress test sessions per week (some of which I was permitted to conduct under supervision) and following the registrar for an average 2 consults per day. I learnt a lot during this time.
Now not everyone has hard cold factual achievements that they can list under their work history. But even something like being praised in a supervisor report for something is better than you just providing a list of responsibilities.
If you have learnt and developed certain skills or capabilities then its also ok to put these down.
My paediatric term in combination with the APLS course I attended helped me to become comfortable in managing sick children.
Don’t forget it doesn’t have to be about your academic work. It could be:
That you managed to get your research project accepted to a peer reviewed publication.
Or that you dedicated extra time to developing up a teaching program in your school. But if you have don’t just say you started a program. How many students did you have? How many teaching sessions did you provide etc…
In terms of extra things. There are a few don’ts or things to avoid.
Don’t put down extra responsibilities without talking about the achievements.
A classic is being a member of a certain committee. If that committee did nothing the year you were on it (as many do). Best not to put this down as you have basically just shown that you like to contribute to inefficiency.
If however that committee fixed something important then take some credit for this.
Putting It All Together
Once you have the content of your Resume pulled together you should first go back and review your personal statement and make sure it fits with the rest of your resume and has all the gems in it.
Then its time to assemble. It’s essential that you compile it in a way that ensures that the most important information is presented first. In particular that you maximise what is on your first page. As this is the page that employers will spend most of their time on.
Things that should go on your first page include:
- Your name, which should be the biggest thing.
- Short qualifications
- Contact details
- Personal statement
- Education history
You may have other things you wish to include but these generally will come on the next pages.
There are lots of options for doing this but either an online CV-builder or a document template will probably ensure that you stick to a simple and professional style and format.
Templates that have 2 columns often work better as they allow you to set out information well but increase what is included on the first page.
In terms of online CV builders here are 3 that we recommend:
VisualCV
Resume.Io
novoresume
A Medical Student Resume Template
Click here to go to a related post where we have a template waiting for you.
Related Questions
Question. Am I limited to listing just one strength in my personal statement?
Answer. No. But you will probably find it hard to provide strengths for all of the criteria. So it’s best to limit yourself to 2 to 3 at the most. Otherwise, you lose their attention and also stop them from focusing on where you want to be. Remember this is determining the narrative that you want them to remember you by. So you have to decide if you want to be known as a medical graduate with a strong research background or perhaps the medical graduate who used to be a management consultant. Try not to confuse them too much.
Question. How long should a personal statement be?
Answer. You should try to make it as brief as possible. Get someone else to read it for you. If you can use one word rather than three go for the one word. As a general rule for a medical graduate, I wouldn’t do more than a couple of paragraphs filling up the top 1/3 of your front page. But its all relative and as you go on further in your career you may want to devote more front-page real estate to your personal statement.
Question. Is there anything I should not put in my personal statement?
Answer. The main thing to avoid is statements or claims that you don’t back up in your resume. For example, if you say that you have excellent clinical skills then you should at least list the key ones you have developed under education. As I say statements such as “a strong focus on high-quality communication” or “strongly valuing teamwork” get quite cliched and grate on experienced employers. Don’t add something in like this unless you can really back up how you have demonstrated it in your career so far.