Preparing for the RACS SET Interview: Your Ultimate Preparation Guide to Interview Training for Surgical Specialties SET Program Selection
The RACS SET Interview selections are arguably the most competitive specialty selection interviews in Australia and New Zealand with only about 1 in 4 to 1 in 5 candidates succesful each year. Having coached over 60 clients to success with the RACS SET Interview Selection I wanted to share with you my tips for your ultimate preparation guide.
What are the RACS SET Interviews?
The Royal Australasian College of Surgeons conducts an annual selection process for selection into surgical training in Australia and New Zealand.
Or to be more accurate RACS in collaboration with its 13 surgical specialty groups or societies conducts 13 application processes each year for Australian and New Zealand trainee doctors to become enrolled in SET selection.
Once selected into training SET trainees face another 5 to 6 years of full time clinical training in hospitals as a SET Registrar prior to qualifying to become a consultant surgeon in their relevant specialty.
What is the Structure of the RACS SET Selection Process?
As an applicant for a surgical training program in Australia or New Zealand you have one opportunity per year to apply for a training position in one or more of the 9 RACS specialties (it is possible to apply for more than one program per year). There are a number of steps you need to undertake in this highly competitive selection which ultimately culminate in appearing for an interview (if successful).
The application process commences in January of each year with a registering with RACS as part of a centralised process. This is essentially an expression of interest as well as a preliminary eligibility check. You must register and pay the registration fee each year that you apply.
What are the Eligibility Requirements for Applying for RACS SET Training?
- You must have Australian or New Zealand Citizenship or Permanent Residency
- You must have general (unconditional) registration with AHPRA or general scope registration with the MCNZ
- You must have completed the RACS Operating With Respect (Anti-Bullying and Harassment) Training Module
- You must have satisfactorily passed the General Surgical Sciences Examination
- There may be additional requirements depending on the specialty you are applying for. Generally there is a requirement to have some surgical experience in the specialty increasingly many specialties are requiring that you pass the RACS Clinical Examination
The RACS application process requires you to submit evidence of your eligibility, contact details for referees and a structured CV.
After registering with RACS you are required to apply for the SET Program/s you wish to apply for.
The next steps vary depending on the specialty. But in general
- Your CV will be scored
- Your referees will be contacted for structured reports
- You may be required to sit a Situational Judgement Test
- Depending on specialty other evidence may me taken into account, such as examination performance
- A final determination of eligibility for interview will be determined
As mentioned at the end of this process, if you are deemed eligible to attend an interview, you will be invited to participate in a semi-structured interview process.
Your final result is then normally determined by a combination of your CV score, reference scores, SJT score (if applicable) and the all important interview score.
More details about the process for 2026 can be found here
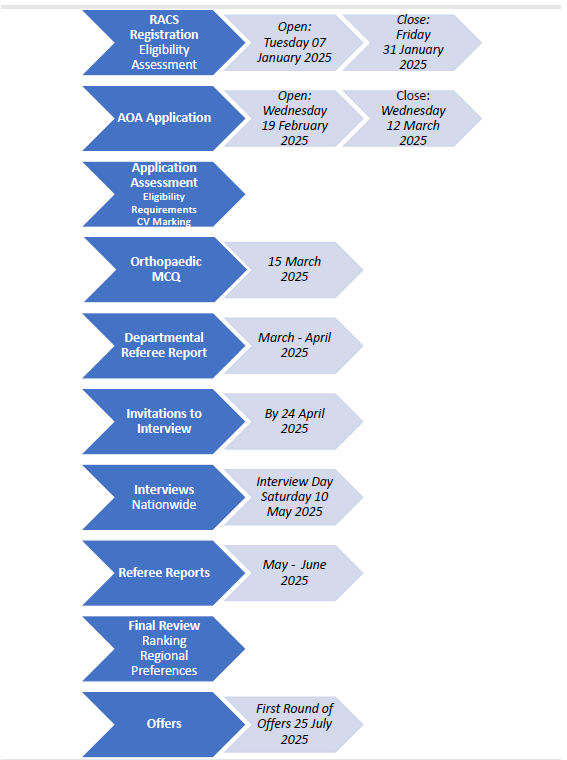
Key Dates for the RACS Surgical Selection Process for 2025
Stage 1: Registration for selection
Opens Tuesday 7 January 2025 (12:00 noon AEDT). Closes Friday 31 January 2025 (12:00 noon AEDT)
Stage 2: Apply to the SET program
The opening and closing dates varies between specialties.
Stage 3: Referee reports collected
April/May 2025
Stage 4: Interviews
The interview dates vary between specialties.
Stage 5: Announcement of offers
Latest day of notification of outcome: Friday 7 November 2025
What is a Semi-Structured Interview?
A semi-structured interview generally means any form of interview with a reasonable amount of pre-planning in terms of the questions and the scoring approach. In the case of the RACS specialties this generally means meeting with more than one group of interviewers (panel members) for a determined amount of time in an interview station. The number of stations vary between 3 () to 8 (). When the number of stations is more than 6 the process tends to be called a Multiple Mini Interview process.
| RACS Specialty | Type of Interview | Number of Stations | Number of Interviewers | Minutes Per Station | Reading / Transition Time | Stem to Read? | Notes |
|---|---|---|---|---|---|---|---|
| General Surgery Australia | MMI | 5 | 2 +/- 1 Observer | 10 minutes | 2 minutes reading time | Yes |
3 Clinical / 2 Non-Technical Stations 2 questions + probing per station |
| General Surgery New Zealand | MMI | 6 | 2 to 3 +/- Observer | 10 minutes | 1 minute reading | Yes | Structured initial question with probing |
| Orthopaedics Australia | MMI | 6 | 2 | 10 minutes | No | Standardised Stem + Probing questions | |
| Orthopaedics New Zealand | MMI | 7 | 3 +/- Observers | 9 minutes | 2 minutes | No | Standardised Stem + Probing questions |
| Plastic and Reconstructive Surgery, Australia | Semi Structured | 3 | 2 to 3 +/- Observer | 15 minutes | No reading time | No | 3 questions per station |
| Plastic and Reconstructive Surgery, New Zealand | Structures | 3 | 2 | 20 minutes | No | Standardised Stem + Probing questions | |
| Otolaryngology Head and Neck Surgery, Aotearoa Australia | Semi Structured | 3 | 2 + Observer | 15 minutes | 5 minutes | Yes | 2 Structured questions + probing per station |
| Otolaryngology Head and Neck Surgery, Aotearoa New Zealand | |||||||
| Paediatric Surgery | MMI | 4 | 2 | No | Clinical + Professional Station / Article Station / Video Review Station / Theoretical Station | ||
| Cardiothoracic Surgery | MMI | 3 | 15 minutes | 5 minutes reading time | Yes | 3 questions per station | |
| Urology | Semi-Structured Interview | 4 | 2 + Observer | 15 minutes | Yes for Sim Pt Station |
1 Sim Patient Station 1 Station specific to either Aus / NZ | |
| Vascular Surgery | MMI | 6 | 2 + Observer | 8 minutes | 2 minutes reading time | ||
| Neurology | Structured | 4 | 15 minutes | Consists of four scenario and experience‐based sections, each with multiple questions designed to assess the suitability of the applicant. |
The above information comes from official information as well as advice from past candidates. You should check each year for changes.
How Can I Best Prepare for the Interview? Tips for Effective SET Interview Preparation
Having now coached around 150 clients through the SET interview challenge I am frequently asked to present on the topic of how best to prepare for the SET interviews. Below are my top ten tips. Some, such as tips 1 – 4, may seem a little obvious but are still worthy of highlighting. Others you may be less familiar with and will hopefully help you to better prepare.
Tip # 1 Give Yourself Plenty of Time to Prepare for the RACS SET Program Selection Process
Most clients start working with me at the start of the year, giving themselves several months to prepare. Some even commence the year prior.
Do you need 12 months to be successful in the SET interviews? No. But its not a bad idea to give yourself that amount of time so long as you pace yourself (see tip 17). Like most performances its hard to improve by cramming a few weeks prior. You will often need time to first deconstruct your approach to answering interview questions and then build new techniques. This takes time and you won’t be sounding smooth and slick straight away.
At a minimum I would recommend at least 3 months to prepare.
Tip # 2 Ensure You Read Carefully Through the Selection Regulations
Make sure you read carefully the selection regulations. Don’t rely on what past trainees say or even what I write here!. Be aware of any updates or changes throughout the year. They are generally revised and updated at least annually. Whilst in general most of the process stays the same, RACS and the specialty groups are always endeavouring to come up with a better process. An example of this has been the introduction of Situational Judgement Tests for certain surgical subspecialties, such as General Surgery, Orthopaedics and ENT in Australia.
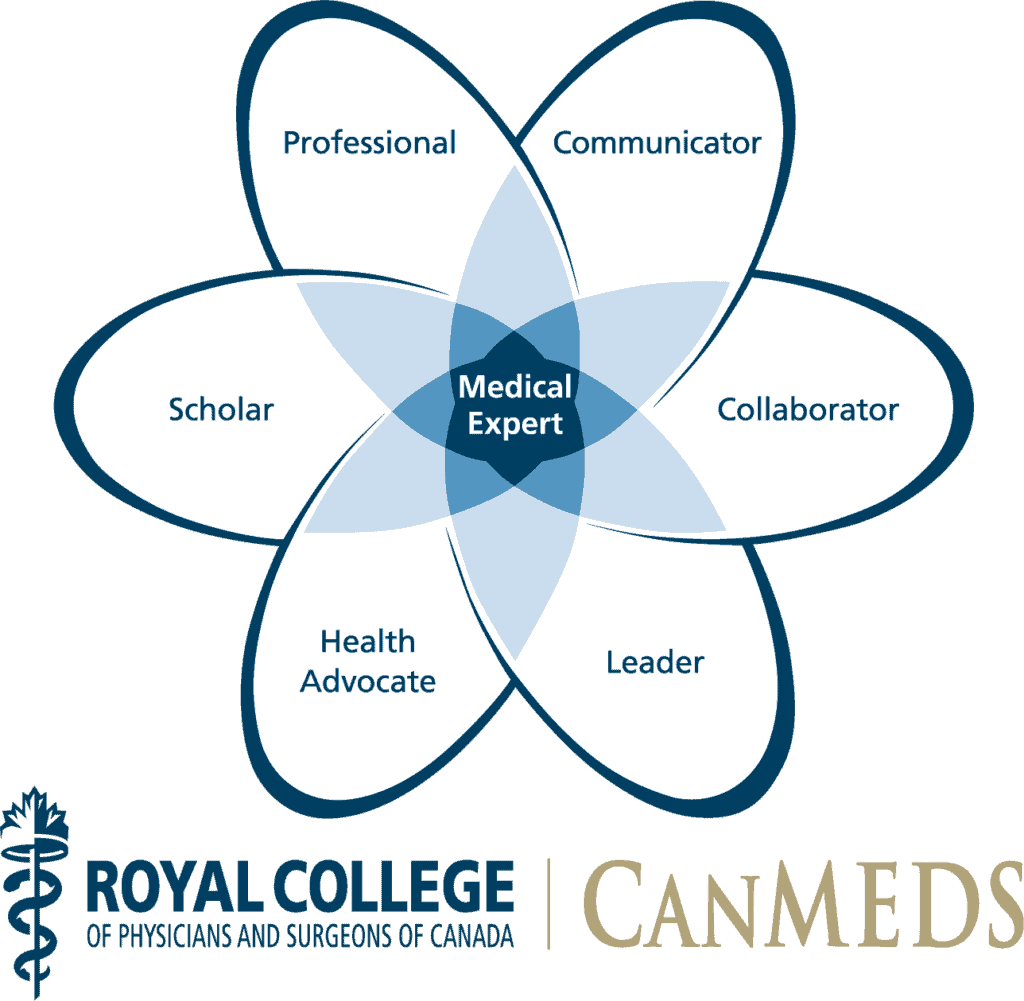
You particularly want to understand what the criteria are for the interview. Generally these are either literally the RACS competencies (based upon CanMEDS) or a variation of these.
These are key to understanding why certain questions are being asked and what is being looked for.
Tip # 3 Don’t Forget Your Registration and to Apply for Selection
Whilst you should be aiming to focus on interview preparation throughout the journey take some time to complete your registration and make payment with RACS and application for selection panels and don’t leave these to the last minute.
Tip # 4 Prepare Your CV Early
As per above get your CV done as soon as possible so its no longer looming over you.
Tip # 5 Make All Points Count on Your CV
I find most clients are pretty comfortable with how to compile their CV to ensure that they obtain the maximum points possible. Most applicants will generally not even bother applying unless they feel that they have a good CV. That being said I am aware of some trainees who successfully challenged their CV score (presumably because things were overlooked).
For this reason I recommend a summary at the start which basically walks the reader through all of your relevant points.
Tip # 6 Choose Your Referees Wisely and Prepare Them
Selecting trainees for interview has become a zero sum game for RACS. Most clients max out their CV points. And most referees are aware that its important to give you a good reference (because every other referee is doing the same).
Still. Its important to be choosy where you can be. Especially if one of your potential referees is more hawkish. But equally important is for you to provide your referees with some reminders of your good past performance. At a minimum give them your CV with some additional information about your achievements whilst you were working with them.
Tip # 7 Invest in the Right Resources for Your Interview Preparation
OK. Now we are getting more focused on the SET interviews themselves.
There’s 3 key types of resources that most trainees will consider investing in for the interviews.
Books, courses and coaching.
Books for the SET Interviews
There are very few Australian or New Zealand books specifically dedicated to the SET interviews. Although many past clients have found the Amanda Nikolic book for General Surgery interviews quite helpful. There are also a range of books from the UK which may provide some assistance.
For SJTs there are actually quite a few books already available written for the RACS SJT. I have not reviewed any of these or heard much about them. So purchase at your own cognizance.
I am not aware of any books with banks of past questions (other than the Nikolic book). The best public repository of past questions is our own one here at AdvanceMed. If you do find this useful then I would ask that you contribute some of your own question after, as many have done before you.
Courses for the SET Interviews
Courses are useful for understanding the theory behind certain interview questions and learning techniques for answering different questions.
There are a few providers who offer RACS SET preparation workshops such as iPrep and IME. IME also offers an online course. At AdvanceMed we have a comprehensive interview skills course which covers off on college interviews. The most powerful sections of this course for RACS applicants are the ones on question frameworks and sign posting. I tend to focus a lot on these sections in my actual coaching. So that’s why the interview skills course is included in my coaching packages.
SET Interview Coaching
You will find quite a few coaches online advertising themselves as being able to help with the RACS SET interviews. For example there’s Claire Berry Consulting and Jo Hely.
As RACS itself says:
RACS in partnership with the Specialty Societies delivering the Surgical Education and Training Program do not accredit, endorse or recommend any commercial providers delivering SET selection and interview training courses.
RACS and the Specialty Societies do not share with commercial providers any information regarding the content and style of SET selection interviews or any other selection tools, and have no evidence of the usefulness of these commercial courses.
So, its important to do your due diligence before engaging with an interview coach.
I am happy to answer any questions that you may have about my own approach to preparing candidates for SET interviews. I would also recommend that you ask around for recommendations from colleagues. Much of my clientelle tends to find me now from word of mouth.
I also offer a RISK FREE Strategy Call where we can see if we are a good fit for each other.
What is Best: Coaching or a Course for Candidate Interview Preparation?
If you can afford it then coaching will by far and away give you better value than an online course or one day workshop.
Nothing beats personal one on one support where the coache is solely focused on your performance and helping you to improve.
Many of the best coaches will have a course built into their coaching program for you as well as other resources. Having coached now for several years I have also built up a library of resources based around key topics that tend to come up in the RACS interviews, for example clinical governance (for which my favourite mnemonic is PIRATES – Patients, Information, Risk, Audit, Training, Evaluation, Supervision) and Artificial Intelligence.
If you are going down the coaching route I would still recommend that you do what most other trainees do which is approach surgeons familiar with the interview process for some feedback sessions as well. Your coach can help you to maximize these.
Tip # 8 Use the Competency Framework and Selection Criteria to Your Advantage
To gain entry into specialty training programs, it’s crucial to use the Competency Framework and Selection Criteria to your advantage. The RACS Surgical Competence and Peformance Framework is an excellent and often overlooked resource that tells you the sorts of behaviours and capabilities RACS is looking for (and not looking for) and is a great touchstone for your interview preparation (as well as SJT prep if you need to sit for this as well).
Some of these competencies are easier to understand and talk about, for example medical expertise, technical expertise and clinical decision making than others such as health advocacy. So give yourself the time to understand all of these and identify examples in your career history of how you have demonstrated all of these. Citing examples is really helpful in the interview and they will often also ask for an example.
I suggest early on making yourself what I call an alignment table, based upon the selection criteria for the interview.
Below is a video example of what I mean.
Tip # 9 Use the Principles of Deliberative Practice
Deliberative practice is a concept first described by Anders Ericsson, which emphasizes the importance of focused, structured, and purposeful practice in achieving high levels of expertise in any field. Unlike regular practice, which may involve mindless repetition, deliberative practice requires individuals to engage in activities that are specifically designed to improve performance. This involves setting clear goals, obtaining immediate feedback, and continuously pushing one’s limits to tackle challenges that are just beyond current capabilities.
Ericsson’s research suggests that deliberate practice is not merely about the number of hours spent practicing, but rather about the quality and intensity of that practice. It involves breaking down skills into smaller components, honing specific aspects of performance, and gradually integrating these components into a cohesive whole. This approach is applicable across various domains, including music, sports, medicine, and education.
Key elements of deliberative practice include:
1. **Goal Setting**: Practitioners must set specific, measurable, achievable, relevant, and time-bound (SMART) goals to guide their practice sessions.
2. **Feedback**: Immediate and constructive feedback is essential for identifying areas of improvement and making necessary adjustments.
3. **Challenge**: Engaging with tasks that stretch one’s current abilities fosters growth. This means practitioners must consistently seek out challenging exercises.
4. **Reflection**: Taking time to reflect on performance and practice sessions allows individuals to internalize lessons learned and strategize for future practice.
5. **Repetition with Variation**: While repetition is crucial, introducing variations in practice conditions can enhance adaptability and skill transfer.
By following these principles, individuals can accelerate their learning and mastery of complex skills, ultimately leading to higher levels of achievement and expertise. Deliberative practice has been influential in redefining how we understand talent and skill development, emphasizing that with the right approach and dedication, anyone can achieve excellence in their chosen field.
How does this apply to the RACS SET interviews? As I have noted above. It’s important to allow yourself time to breakdown the interview into its smaller elements.
If we think about one MMI station. Within this station you will have somewhere between 2 to 6 questions to answer. Each question is in itself a mini part of the performance.
And answering each question can be broken down into elements, including:
- reading and or hearing the question
- clarifying the question (if needed)
- starting your answer – see below
- expanding on your answer
- completing your answer
- handling any follow up or probing question
Deliberative practice suggests that we should try to focus on the hardest part of the task. For most clients this tends to be the start of the answer. This is why I tend to focus a lot on what I call “sign posting:.
Tip # 10 Practice “Sign Posting” Your Answers
Sign posting is about ensuring that the opening part of the answer to each question is clear and gives yourself and the listener (panel members) a clear understanding of the direction you intend to take.
A well constructed sign post can do many things, including:
- Give you and the panel members immediate confidence (make a good first impression).
- Ensure you have identified all the key components of the question (have a good list of issues).
- Prevent the panel members interrupting you unnecessarily, as they will understand what you intend to cover.
- Mitigate against you running out of time to discuss certain points.
Tip # 11 Make Sure You Identify All the Issues
Its really important that you identify all of the issues in a question.
Oftentimes I see clients dealing well with the clinical aspects of a question but ignoring the more longer term or downstream issues, such as clinical governance issues or opportunities for you to reflect on your own practice or opportunities for quality improvement.
As a bit of a rule I recommend that when you practice you should be targeting 4-6 issues per question. This is not a set in stone rule. But generally when clients are generating 1 to 3 issues they are missing something important.
Being able to identify a less obvious issue may very well be the difference between a good performance and an outstanding performance on that question. And given the competitive nature of the SET interviews you are really wanting to get as many outstanding performance results as possible.
Tip # 12 It’s OK to Question the Question
You are applying to become a surgeon. Which means thinking for yourself. Don’t always take the question as literal and watch for traps or twists. Have you considered every word in the question – why did they include that bit of information? Is there some obvious information missing.
Here’s an example from a past question.
You are seeing an elderly man from a Non-English Speaking Background. His test results have just come back and it turns out that he has cancer. His family requests that you not inform him of the diagnosis as they feel it will unnecessarily upset him.
What would you do?
Most doctors when they see this question begin by outlining how they have identified issues in relation to:
- dealing with ethical issues around autonomy and the right to know
- planning treatment for the cancer
- working with the family in the best interests of the patient
- engaging with an appropriate interpretor
- involving the consultant
All great points.
But overlooked here is the question as to why the family knows before the patient? Is there a capacity issue or has there been some form of breach of privacy?
On this point. It’s okay to respectfully challenge the premise of the question by suggesting more information would be useful. Just be prepared to back this up with what that information is.
Tip # 13 Adopt a Surgeon’s Mind Set
This tip is a little bit complex to explain in a blog. It goes hand in hand with the above tip. It’s a kind of you know it when you see it and hear it sort of thing. Your aim is to try to think and talk like a surgeon, or at the very minimum a seasoned SET trainee in the specialty you are aiming for.
Think of your most trusted surgical mentor. Who is that person that you regularly go to for advice? And when you do go for advice. Do they just give you the answer or do they take a step back and as a number of really insightful questions first? The latter is who you are aiming for.
What you are wanting to avoid is narrow thinking. Don’t approach a question as if you are who you currently are, which is likely to be an unaccredited registrar or SRMO. If you answer from your current perspective you will tend to overlook all the extra tasks that a good surgeon or SET trainee would be expected to accomplish.
Tip # 14 Get the Right Feedback
There’s good feedback and unhelpful feedback. Good feedback should follow the principles of effective feedback, by which I mean it should be specific, clear, relevant and delivered as soon as possible.
Who is providing the feedback is also important. You are not going to get very helpful feedback from family, friends or colleagues. Even some consultants will be of little use to you.
Its important to try to obtain feedback with someone who has had experience with the process. This effectively means surgeons who have been on selection panels in previous years (possibly some registrars who have successfully navigated the process) and coaches who have the experience to know what works best for clients.
Sessions with an experienced consultant surgeon are often gold. Because they are generally only offered a few times each year. Make sure you make the best of these by being clear and explicit about what sort of feedback you are seeking. The well meaning consultant may be keen to get through as many questions as possible. This is not going to help you as much as them providing one or two “gems” or insights by helping you focus on specific aspects of your performance, such as your opening approach.
Tip # 15 Record Yourself
When I coach clients for interviews I exclusively do this online. There’s a number of reasons for doing it this way. But one advantage is that we can easily provide a recording of the session, which I do for all of my clients. Those that do watch the videos tend to be more successful than those who do not.
I strongly encourage you to record your practice sessions. If you are not doing this then you are missing out on lots of valuable and immediate feedback. You will be able to assess your tone and pace of voice, your body language, and pick up on bad words to avoid. And your competitors are doing this, so you are placing yourself at a disadvantage.
Tip # 16 Regular Practice is Better than Intense Practice
The next 2 tips also go together.
Consistent with deliberative practice and general principles for improving and sustaining performance you want to be performing regularly not necessarily quantitatively. You can only learn and adjust a few things in one practice session before reaching cognitive overload. So there’s no point practicing for several hours.
You can actually achieve quite a bit with a half hour practice session. And if you are prepared (with a bank of questions and recording option) you can even sneak a session into your break or downtime at work.
At this time of the year I am generally recommending to my clients that they try to practice 30 to 60 minutes per week, twice a week. That’s enough at this stage. As you get closer to the interview you will likely want to increase the intensity. And that’s okay because you will have left yourself the energy and drive to do so.
Tip # 17 Don’t Peak Too Early – Avoid Burn Out
As I have mentioned previously. It is important to time your practice so that it is regular and not overly taxing during the months beforehand. As you get closer to the interview time you are going to want to increase the intensity of your practice.
If you feel yourself getting frustrated weeks or months before the interview. Give yourself a bit of a break. Don’t burn out.
With my clients I aim for them to peak by feeling something between ready for it and a bit frustrated (wanting to get on with it) a week or so prior.
Tip # 18 Optimize Your On the Day Performance Early
By this tip I mean get all the logistics out of the way. Book your leave as soon as possible. Make sure you feel comfortable in your suit and that its dry-cleaned.
If you are doing a video interview make sure your room, technology, lighting etcetera are optimised. See this post for a guide on video interviews.
If you are attending in person, book your flights or travel. Book your hotel room. If interviewing in another city try to arrive a day or two earlier if possible. If you haven’t visited the site previously try to check it out in person a day or two beforehand so you know exactly where to go. I recommend booking a taxi or Uber for your travel rather than worrying about using your own car and finding a car space.
If you have followed my recommendations about how to prepare then I don’t actually recommend doing much practice the day or two beforehand. It’s not going to do anything for you. Instead try to relax, whatever way works for you. Book a massage. Definitely go for a walk, run or swim. Have some nice food. Try to get some decent sleep. Treat yourself.
Tip # 19 Remember Each Station or Panel is a New Chance to Make a Good Impression
Some surgical specialties are quite small so you may have a consultant on a panel that knows you already. But generally the panel members have not met you before and don’t know your history or background. With an MMI process there is generally no discussion of candidate performance between panel members either.
This has certain implications:
- Each new panel is another chance to make a good impression.
- If you feel like you had a bad station. The next station is a fresh chance to recover.
- You can use the same example in different stations.
- Try to give each panel some information about your career in order to give them confidence that you would be a safe pair of hands if you were their registrar.
Tip # 20 Have a Plan B
Not everyone is succesful in gaining a SET training place. This does not mean that you are a failure or that you would not make a good surgeon. Just to be eligible for an interview puts you in a rare cohort of trainee doctors and I can’t recall a single client who I felt would not make an effective trainee. There is a degree of luck in this process.
Because you have invested so much you may be falling victim to the sunk cost fallacy. At a certain point its important to consider and identify another training option. In fact, doing this may just take the pressure off and I have seen this leading clients getting into surgical training.
What are the things you like about surgery and how might this transfer into another career in another specialty or even a creative career?
You may want to spend time with a career coach discussing this and identifying other options. Once you have decided on another option you may also want to discuss how this affects your CV and application process.
Tip # 21 Thank Your Family and Friends
At the end of this, likely, several month process, your family and friends have been cheering you on and wishing you the best. You have probably ended up spending less time than you would wish with them. Nows the time to thank them and pay them back.
Notes on Surgical Education and Training Selection by Specialty
General Surgery
Australia
With the introduction of GSET, the training program has moved to a five-year program for all trainees who commenced from 2022 onwards.
Based on modelling through analysis of the above factors, the current predictions indicate that the 2025 selection process (for 2026 intake) will see fewer offers than usual being made, based on current Trainees exiting the program.
Approximately 30 spots will be available for the 2026 intake (significantly less than normal).
It is anticipated that in 2026 (for 2027 intake) the number of offers will revert to normal.
| Rotation Type | Minimum Duration |
| General Surgery Rotation | 26 weeks |
| Critical care rotation | 1 X 8 weeks |
Applicants must submit the completed Australian Board in General Surgery Procedural Skills and Professional Capabilities Form available on the GSA website.
New Zealand
Applicants must have successfully completed the Royal Australasian College of Surgeons Generic Surgical Sciences Examination (GSSE) prior to the Specialty application closing date, in addition to having a minimum of 52 weeks General Surgery experience which must be completed by the time of application.
A completed Procedural Skills and Professional Capabilities Form which shows validation by a supervisor of a number of professional activities and operative procedures is also required. The procedures must be verified during rotations taken in the twelve (12) months prior to the closing date of applications.
Selection Timetable 2025
Selection Registration Opens – 7 January 2025
Selection Registration Closes – 31 January 2025
Selection Applications Open – 4 March 2025 – 2.00pm
Selection Applications Close – 25 March 2025 – 2.00pm
Referee Reporting Opens – 29 April 2025
Referee Reporting Closes – 27 May 2025
Interviews – 18 June 2025 in Wellington
First offers made – 1 July 2025
Last date for Offers – 7 November 2025
Orthopaedics
Australia
Orthopaedic Multiple Choice Question (OMCQ) Test
The 2026 Selection Intake process will include completion of an OMCQ Test. More information on the OMCQ can be found on the OMCQ test information sheet.
New Zealand
Stages of selection and key dates
- Registration Opens 12pm AEDT: Tuesday 7 January 2025
- Registration Closes 12pm AEDT: Friday 31 January 2025
- Applications Open 12 noon AEDT: Wednesday 19 February 2025
- Applications Close 12 noon AEDT Wednesday 19 March 2025
- Workplace Assessments Open 9.00am AEST Wednesday 16 April 2025
- Workplace Assessments Close 8.00pm AEST Wednesday 30 April 2025
- Interviews will take place in New Zealand on a date and place to be determined and advised.
Urology
Eligibility
- Applicants must also have passed the Clinical Examination (CE) by the application closing date.
- Complete a minimum 26 weeks in Surgery in General at PGY2 or above by the application closing date.
- Complete a minimum of 10 weeks in Emergency Department (ED) at PGY1 or above by the application closing date.
- Complete a minimum 26 weeks in Urology at PGY2 or above by the application closing date.
Registration
Any person intending to apply for selection to the Surgical Education and Training Program in Urology must first register in accordance with the RACS Regulation: Registration and Selection to Surgical Education and Training. Applicants who have not registered cannot lodge an application for the Surgical Education and Training Program in Urology.
Registration is completed online on the RACS website. Registration fees apply.
The Registration Period for the 2026 intake (conducted during 2025), is:
- Registrations Open Tuesday 7 January 2025 at 12:00 noon AEDT
- Registrations Close Friday 31 January 2025 at 12:00 noon AEDT
Late registrations will not be considered.
Application
Applications may only be submitted by registered applicants using the online Urology Application form.
Applicants will be required to pay an application fee to be considered for selection. This fee is non-refundable and must be paid prior to the closing date. Failure to pay the application fee by the closing date will result in the application being withdrawn.
The Application Period for the 2026 intake (conducted during 2025) is:
- Applications Open Wednesday 19 February 2025 at 12:00 noon AEDT
- Applications Close Friday 21 March 2025 at 12:00 noon AEDT
During this time, eligible registered applicants will be able to access an online application form. Late applications will not be considered.
Referee Reporting
The Referee Reporting Period for the 2026 intake (conducted during 2025) will be from Monday 21 April 2025 until Friday 23 May 2025 (approximately).
Interviews
Interviews for all shortlisted applicants will be held on Saturday 14 June 2025. Interview locations will be communicated when finalised.
Vascular Surgery
Vascular Surgery Selection Eligibility
In addition to the RACS generic eligibility criteria applicants must fulfil the following specialty
specific eligibility criteria:
- Successful completion of RACS Generic Surgical Sciences Examination (GSSE) by date of
application. - Successful completion of the Clinical Examination by date of application.
- 8 weeks full time surgical rotation in General Surgery undertaken within the 7 years
immediately prior to, and completed by, closing date of application. - 16 weeks full time surgical rotation in Vascular surgery undertaken within the 7 years
immediately prior to, and completed by, closing date of application.
No more than two rotations of at least four weeks can make up the minimum requirement for the surgical rotations. Vascular rotations must have at least two (2) Fellows of RACS (FRACS) employed as a specialist surgeon; or one (1) vocationally trained surgeon employed as a specialist surgeon who works at the hospital on a weekly basis and one (1) FRACS employed as a specialist surgeon.
Applicants may apply to the BOVS Chair in writing at vascular.selection@anzsvs.org.au for an extension to 6.1.1c and d for interruptions due to family leave or other personal circumstances, e.g. illness, research, or higher degree.
Rotations indicating leave cover, relief, or shift work will not meet the requirements.
Rotations indicating Private Assisting will not meet the requirements
Rotations in part time positions will count towards the requirements on a pro-rata basis of a full-time position. For example, working 19 hours per week for 8 weeks will calculate to 4 full time weeks.
Plastics and Reconstructive Surgery
Australia
Key Dates for 2025:
- Selection Registration Opens (RACS) Tuesday 7 January 2025 12:00pm AEDT
- Selection Registration Closes (RACS) Friday 31 January 2025 12:00pm AEDT
- Selection Application Opens (ASPS) Monday 24 February 2025 12:00pm AEDT
- Selection Application Closes (ASPS) Monday 24 March 2025 12:00pm AEDT
- Referee Reporting May 2025 (evenings Mon-Thu)
- Interviews (virtual) June 2025 – all conducted virtually mid-week. Day TBC
- Last Date for First Round Offers Friday 25 July 2025
- Last Date for Final Offers Friday 7 November 2025
New Zealand
SET Selection timetable 2025
- Selection Registration opens – Tuesday 7 January, 12 noon AEDT
- Selection Registration closes – Friday 31 January, 12 noon AEDT
- Selection application opens – Wednesday 19 February
- Selection application closes – Thursday 27 March
- Referee reporting opens – Thursday 24 April
- Referee reporting closes – Wednesday 21 May, 8pm AEST
- PRS Interviews: Thursday 19 June, Wellington
- Last date for first round offers – Friday 25 July
- Last date for final offers – Friday 7 November
Otolaryngology Head and Neck Surgery (Ear Nose and Throat Surgery)
Australia
Selection: Key Dates for 2025
- Selection Registration Opens Tuesday 7 January 2025
- Selection Registration Closes Friday 31 January 2025
- Selection Application Opens Wednesday 26 February 2025
- Selection Application Closes Thursday 20 March 2025
- CV Score Notification Thursday 3 April 2025
- Referee Reporting and Multi-Source Feedback Collection April/May 2025
- Referee Reporting and Multi-Source Feedback Score Notification by Friday 30 May 2025
- MMI Interview Notification by Friday 30 May 2025
- MMI Interviews Saturday 14 June 2025
- Latest Date of First Round Offers by Thursday 10 July 2025
- Last Date of Offers Friday 7 November 2025
The selection process uses four selection tools, each contributing a weighted score as:
- Structured Curriculum Vitae 15%
- Multi-Source Feedback 10%
- Structured Reference Reports 35%
- Semi-Structured Interview 40%
Only the top ranked suitable applicants will progress to the interview stage. The number of applicants interviewed will be based on estimated number of positions available in 2026.
New Zealand
Cardiothoracic Surgery
The Selection Process reflects the bi-national nature of the Training Program and is open to Applicants from both Australia and Aotearoa New Zealand.
The Training Program is overseen by the Committee across both Australia and Aotearoa New Zealand. Successful Applicants must be prepared to be allocated to a Training Post in either of those two jurisdictions for any rotations during their training, recognising that breadth of experience obtained across a variety of Training Posts is likely to help meet the goals of the Training Program. Applicants are expected to have a commitment to equity of health outcomes and understand issues that face marginalised and disadvantaged groups within our communities.
Neurosurgery
Key Dates
- Registration Opens for the Neurosurgery Anatomy Examination: 12 noon AEDT Monday 11 November 2024
- Registration Closes for the Neurosurgery Anatomy Examination: 12 noon AEDT Monday 9 December 2024
- RACS Selection Registration Opens: 12 noon AEDT Tuesday 7 January 2025
- RACS Selection Registration Closes: 12 noon AEDT Friday 31 January 2025
- Neurosurgery Anatomy Examination: Friday 21 February 2025
- Neurosurgery Selection Applications Open: 12 noon AEDT on Monday 3 March 2025
- Neurosurgery Selection Applications Close: 12 noon AEDT on Monday 24 March 2025
- Interviews for shortlisted applicants: Thursday 26 June 2025
- Release of Offers: Prior to 5pm AEST on Friday 27 June 2025
The selection process uses four selection tools, each contributing the following weightings to the overall selection score out of 100:
- Neurosurgery Anatomy Examination 30%
- Structured Curriculum Vitae 10%
- Reference Report 30%
- Neurosurgery Semi-Structured Interview 30%
Paediatric Surgery
Paediatric Surgery Selection Criteria
The SET Program is conducted by the Committee across both Australia and Aotearoa New Zealand. Successful Applicants must be prepared to be allocated to a Training Post in either of those two jurisdictions. The Selection Process reflects the bi-national nature of the SET Program and is open to Applicants from both Australia and Aotearoa New Zealand.
- Applicants are expected to have a commitment to children’s health and wellbeing and understand how that requires different considerations to health systems designed to deliver care to adults.
- Applicants are expected to have a commitment to equity of health outcomes and understand issues that face marginalised and disadvantaged groups within our communities.
- Applicants are expected to have demonstrated capacity to deal with paediatric patients and their families.
- Applicants are expected to have some experience with operating on children and infants. 2.3.7 Applicants are expected to have competency navigating medico-legal and ethical issues surround delegated consent to parents or legal guardians and tensions that can arise when there is conflict between carers and/or the interests of the child.
- Applicants are expected to have a reasonable level of understanding of normal growth and development and be able to identify the significance of deviations from norms.
- Applicants are expected to have an awareness of the potential for non-accidental injury and must understand local jurisdictional responsibilities related to identification and reporting.
- Applicants must have knowledge and experience in managing the psycho-social implications of illness and hospitalisation for children and their families.
Related Questions
How many candidates are successful in Australia and New Zealand each year?
Answer. Success rates vary from year to year. RACS publishes an annual activities report where you can track competition ratios. The latest report available is the 2023 report (which reports on the 2023 selection process for 2024 commencements).
You can see for 2023 competition ratios varied from 11.5% for Cardiothoracic Surgery to 50.0% for Urology with an overall success rate of 31.5%
How Many SET Positions Are Available?
Again, numbers vary from year to year. Some of the smaller specialties may not even offer interviews in some years.
According to RACS there were 1269 active surgical trainees in 2023
What are the dates for RACS Selection in 2026?
These dates are generally determined towards the end of the previous year.
Where can I find past questions to practice with?
The best collection is the AdvanceMed QuestionBank