One of the most frequent questions I receive from doctors from overseas is “How do I get into residency training in Australia?” Becoming a specialist doctor is generally a very rewarding pathway, which can afford a lot of independence and financial stability and is probably the ultimate aim of most doctors in Australia
So I have put this post together as an overview of how this all works. In so doing I wanted to make a few key points:
1. The process of becoming a specialist doctor in Australia is termed “specialty training” and in most cases is conducted via one of the 16 specialist medical colleges.
2. Residency training, which is often what doctors from places such as North American and Asian countries refer to when they are talking about specialty training, does not exist as a concept in Australia. And in fact, being a “resident medical officer” means something quite different here.
3. There are around 64 different medical specialties to choose from in Australia, and this includes general practice, which is recognised as a specialty in its own right.
How and when do local graduates enter into specialty training?
Medical school has been rapidly evolving in Australia of late with the majority of schools phasing out the old MB BS programs in favour of 4 or 5 year MDs. Some of these are graduate programs. So its not surprising to hear that for some the process of choosing and targeting a particular specialty begins early in medical school.
However, unlike say the North American system you can’t simply apply for specialty training at the end of your medical school.
Upon graduating there is a requirement for a minimum of one year supervised training which is referred to as an “internship”. It is only after you satisfactorily complete your internship that you gain general registration. Doctors from the United Kingdom and the Republic of Ireland would be familiar with something similar. The Australian medical training system has largely been adapted from the UK system.
The internship period is heavily supervised and there are a formal training and assessment processes, with oversight provided by bodies in each State and Territory called Prevocational Medical Councils.
This prevocational period often extends for at least another year and we call it prevocational training.
Resident Means Something Different in Australia.
A Resident or Resident Medical Officer, or RMO in Australia is a doctor in their second year out of medical school, i.e. someone who has completed their internship.
Whilst it is technically possible to enter into some specialty training programs as a Resident (Psychiatry and General Practice being examples) generally most doctors wait until the end of their second year to enter into training. And in the case of some particularly competitive specialties, such as surgical specialties and anaesthesia, may wait several more years to get on to a training scheme.
A doctor who is still a resident in their third year is generally referred to as a Senior Resident.
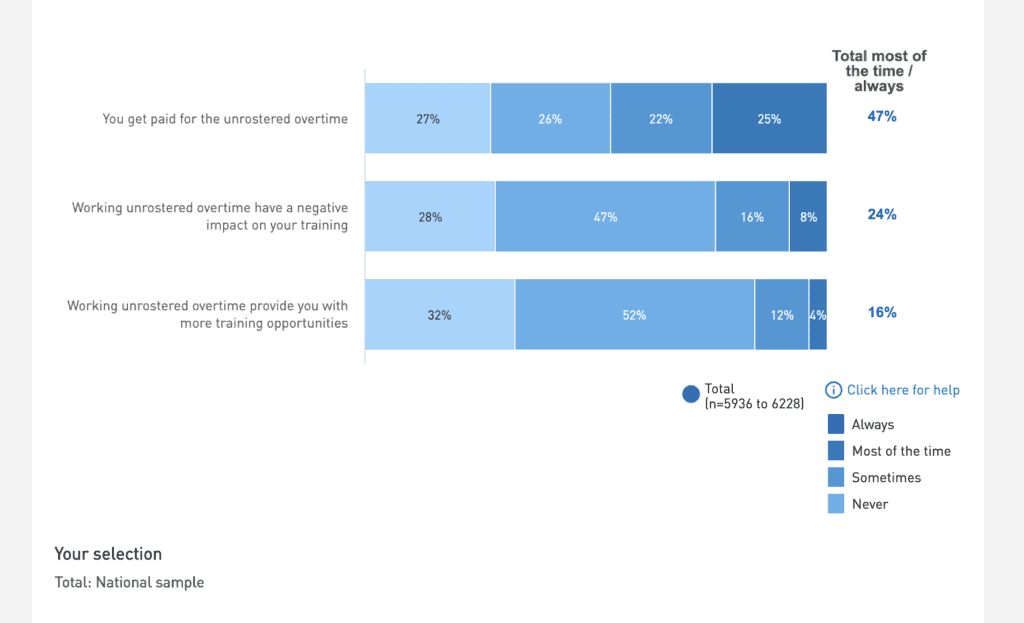
For most senior resident doctors, there is no set standard or oversight for training. So the quality of support provided can vary quite considerably. And it can often be left up to the individual to develop their own program. This situation has unfortunately led to some fairly famous recent cases of exploitation of doctors working what are termed “unaccredited posts”. These are posts that are not oversighted as an official training post by a college. Often referred also to as service roles.
It’s for this reason that doctors in Australia are often relieved when they finally make it into a specialty.
For International Medical Graduates coming via the standard pathway or in some cases also the competent authority pathway. Its a Resident post that you are looking to fill as your first job in Medicine in Australia, i.e. a pre-specialty training position.
Key Requirements for Specialty Training.
The requirements for entry into specialty training differ between colleges and this post is not intended to address each one specifically. But let’s look at some of the general requirements.
You Must Have General Registration to Enter Specialty Training.
One thing that every doctor must have to enter into specialty training in Australia is general registration. So for local graduates, this means completing an internship first. For IMGs this means completing a provisional year, normally as a resident, either via the standard pathway or competent authority pathway, after which you will also be granted general registration.
This is why I often tell IMG candidates that once you have completed your supervised year you are almost on an equal footing with local graduates.
You Generally Need at Least 2 Year’s Experience.
Most but not all colleges require you to have gained a minimum amount of clinical experience prior to applying. The most common requirement is for 2 years.
Whether this is a valid requirement or not is somewhat questionable. As noted some colleges now allow doctors to apply after completing an internship.
A key driver for maintaining a second-year residency in Australia is the need for doctors to fill service level roles. But to be fair many doctors themselves also value having 2 years to consolidate after medical school.
Having Permanent Residency Or Citizenship Can Also Be A Requirement.
In some cases, for example, the Royal Australasian College of Surgeons, you will also need to prove that you are a Citizen or permanent resident. So this can be a discriminator against IMG doctors.
I am often asked why there is this discrimination in place. To be fair to the colleges they are really only applying the Australian law which essentially dictates that jobs must be provided to citizens and residents first before being offered to someone on a visa. Many other countries have similar arrangements for their own citizens.
The Application Process Itself.
The application process itself is similar to a normal job recruitment process. There are 2 main ways to get selected into specialty training in Australia.
1. College Goes First.
The first way is to get selected by the College first. This is the approach that most Colleges adopt. Examples, include RACS, RANZCO, RANZCOG and RANZCP.
For trainee doctors, this selection process may be the most rigorous job interview that they ever encounter, with many colleges employing scoring criteria for both your CV, as well as referees and submitting candidates to psychometric testing and a multiple mini interview approach.
There is often a fee of several thousand dollars to apply with no refund if you don’t make it!
After the college has selected which candidates it prefers for training the employers (the hospitals) may invoke their own second selection process or just accept the finding of the college.
2. Employer Goes First (Alone).
If you are applying for Physician training or Radiology training then you will start off by interviewing for a training post which is held by a hospital or health services. This will generally be a more standard affair, with an online application, CV and referee checks and interviews. Normally its just a panel interview but there has been a trend lately to making some of these recruitments multiple mini interviews.
There will generally be representatives of the respective college on the selection panel.
Once you have gained a post you will apply to be recognised as a trainee by the relevant college. In the case of Physicians, you can even do this beforehand. The process is generally just an application and fee and rarely are doctors rejected.
General Practice Selection.
General Practice Selection is a whole beast to itself, with many pathways.
The main pathway into GP training is conducted by the regional training providers, which are separate from the GP colleges. Selection is quite rigorous and also involves both psychometric testing as well as formal interviewing. Once selected, candidates then apply for one or both other College training programs for which they have already been deemed eligible bypassing the training selection process.
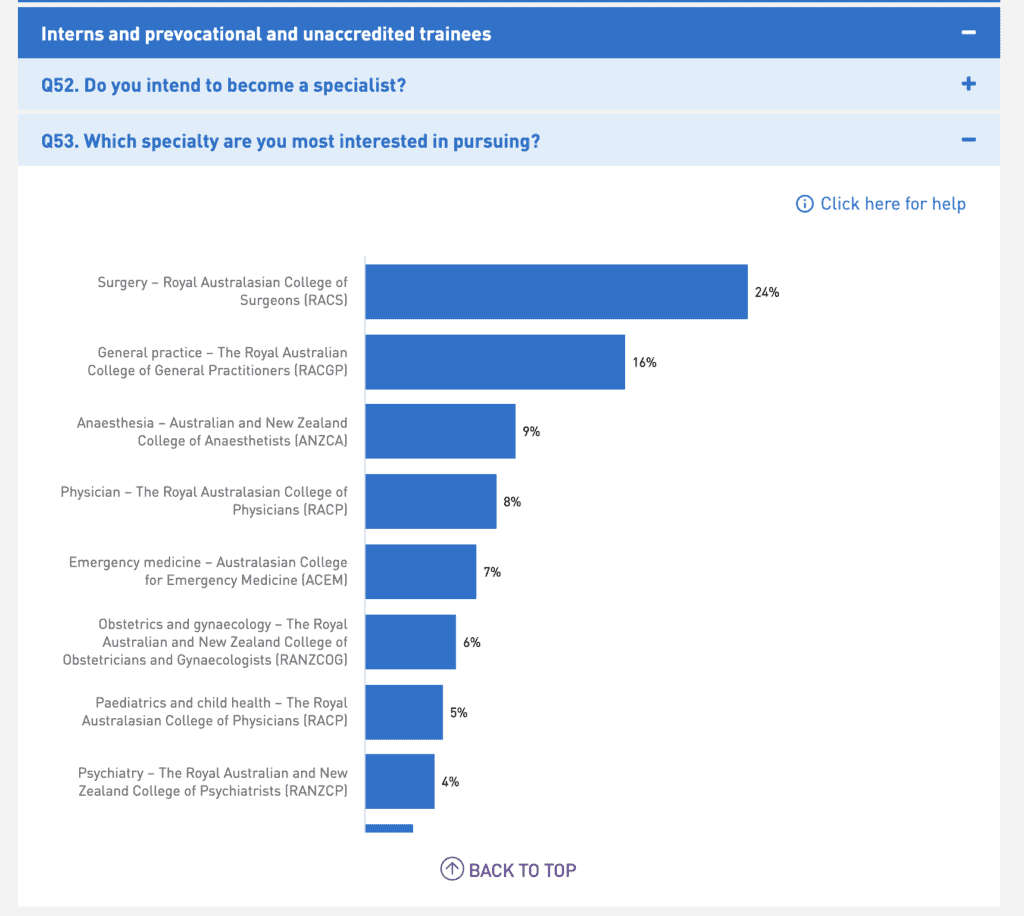
What Specialties Can You Apply For?
If we take the latest view from the Medical Board of Australia there are 64 recognised specialties for medicine in Australia. And below that many hospitals and employers will recognise even more subspecialties.
That seems a lot of choices. But actually the initial choice is made a little bit easier by virtue of the fact that many specialties break their training up into Basic and Advanced Training. Basic Training is usually around 2 or 3 years and more generalised. Once you complete Basic Training you can specialise further in Advanced Training. Which usually requires you to undertake an additional selection step.
Let’s look at some of the more popular specialty choices in Australia.
For General Practice. As indicated there are a number of pathways but the main pathway is the Australian General Practice Training Program under which you train for a Fellowship with either the Royal Australian College of General Practitioners or Australian College of Rural Remote Medicine.
For both Adult Medicine and Paediatrics you commence Basic Training with the Royal Australasian College of Physicians. After which you can choose to stay general in your Advanced Training or do one of many different specialties. The RACP also looks after some other smaller training programs, including Occupational Health and Rehabilitation Medicine.
For Radiology, you apply to the Royal Australian and New Zealand College of Radiology. This is a relatively straight forward specialty. There are really only two options. Diagnostic Radiology and Radiotherapy.
For Psychiatry, you apply to the Royal Australian and New Zealand College of Psychiatrists.
For Emergency Medicine, it’s the Australasian College for Emergency Medicine.
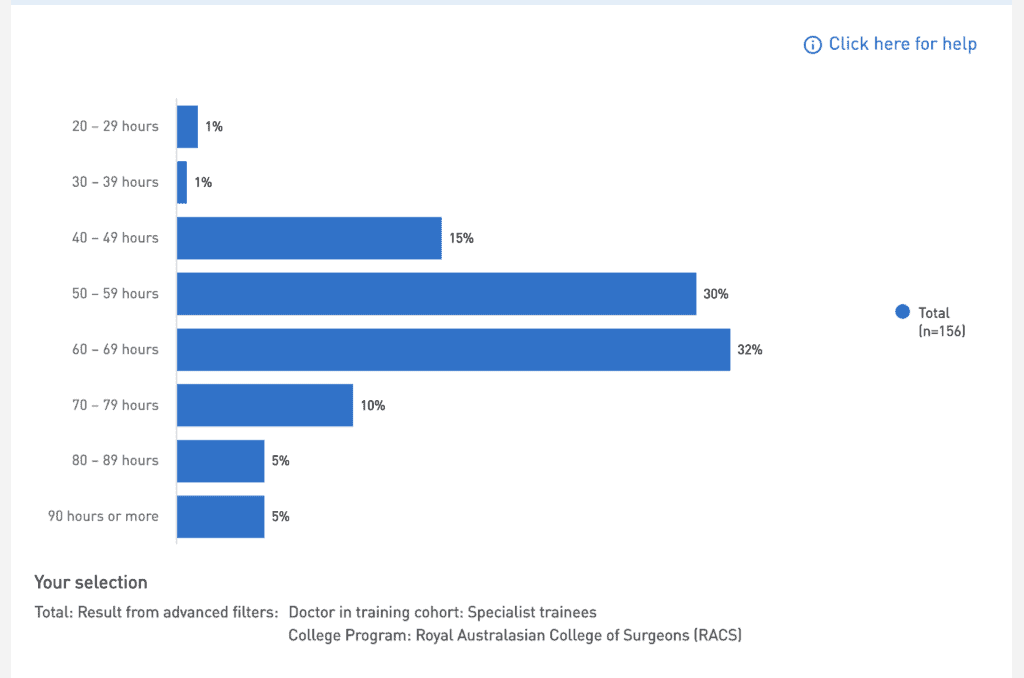
Surgery is a little different. Because its such a competitive specialty trainees have generally completed a lot of experience and courses just to get in. So you apply directly for “SET” (Surgical Education Training) in either of General, Vascular, Orthopaedics, Ear Nose and Throat, Paediatrics, Cardiothoracic, Neurosurgery, Urology or Plastic Surgery.
We have a more detailed post about the Specialty Colleges here.
Other Related Questions.
How Long Does Specialty Training Run For?
Do You Get Paid When Training?
How Do You Enter Training Via the Competent Authority Pathway?
What post you are able to fill will largely depend on your current level of experience and training. If you have just finished Foundation Year in the UK then you will probably only be able to apply for Resident level jobs.
But let’s say you have almost finished your Residency in Anaesthetics in the US. Then you will probably be permitted to fill an unaccredited Anaesthetic Registrar post. But not something that you are not experienced in, such as a Psychiatry post.
Once you have completed your 12 months supervision successfully you can apply for general registration, after which you can apply to enter training in Australia. You may be eligible for some recognition of prior learning.