Category: Blog
Our Doctor Career & Medical Job Blog
Come back regularly as we endeavour to give you the most comprehensive information on the doctor job application process. All things medical job-related.
-
How to Deal With Bullies In Medicine. 8 Tips For Surviving.
Recently a trainee doctor left me a message on the website asking for some help with dealing with a number of senior colleagues who were bullying them in the workplace. Unfortunately, he or she did not leave any contact details. But given that this is certainly not the first time I have been asked for help in this manner I thought it would be a good idea for me to share some thoughts on the subject of how to deal with bullies in medicine.
I want to make this a practical post for any of your struggling with dealing with difficult behaviour in the hospital or community medicine. I’m more than happy to write an article on the causes or potential solutions to bullying and in fact, have done so in the past. But this post is for those of you already immersed in the problem with no hope of a rapid culture change program to bail you out right now.
So here are a few practical tips for things you can do or try if you are encountering a bully in medicine. You can:
- use distance to avoid the doctor bully
- dodge and avoid encounters with the doctor bully
- slow down the rhythm of encounters with the doctor bully
- become invisible to the doctor bully
- find someone who can act as a “bully blocker” to the doctor bully
- tag-team with partners to deal with the doctor bully
- find or establish safety zones for recovery from the doctor bully
- establish an early warning system to avoid doctor bullies
I do however emphasise that this is a list of tactics for dealing with the acute issue of a bully in the workplace. For long term problems, there is a need for a more systemic approach. But given that hospital cultures often take years and many trainee doctors rotate every 10 to 26 weeks or so, some practical tips are justifiable.
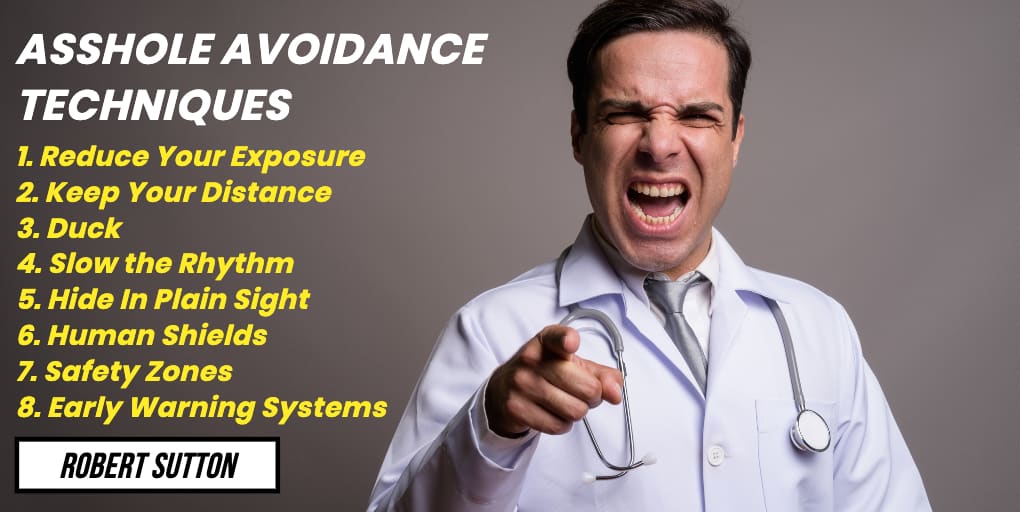
So let’s explore these tips one by one in more detail below.But first, let’s credit the source of inspiration which is Professor Robert Sutton who is, in my opinion, the world’s leading authority on workplace bullies or what he terms “assholes”. He has written a number of books on the topic all of which I would highly recommend. But the inspiration for this particular article comes from one of his later books. The Asshole Survival Guide.
Tip 1 Keeping Your Distance From Bullies in Medicine
This may seem obvious but most places where we work in Medicine afford us a fair deal of space. As Sutton points out in his book generally the closer you are to someone in the workplace the more often you communicate. Which is great if you get on with that person, but if that person is a bully then closeness is a bit of a problem. You may not be able to get the bully to move away from you but perhaps there are opportunities for you to move a bit further away to avoid being in the line of fire?
For example, can you move desks or change your presence in the ward round line? Maybe rather than accompanying them in the lift, suggest you are happy to wait for the next one or take the stairs instead. Or rather than sit opposite them in a meeting, sit on the same side of the room but a few chairs down so that its harder to make immediate eye contact?
If you are in some sort of position to get the bully themselves to move you might try to the trick that a few university professors used to move on a rather pompous colleague. They offered the colleague a new and better office away from the main campus and the colleague took the bait and was rarely seen again.
Tip 2 Dodging and Weaving Bullies in Medicine
This next tip may take a bit of creativity. But if you think about it there are often all kinds of reasons not to be near a bully when you are working in a hospital or other health care environment. Perhaps a sick patient needs to be urgently reviewed. Perhaps there is a relative that needs to speak with a doctor. Perhaps you can be off collecting the XRays for the XRay meeting (OK yep I know these are mainly on the computer these days but you get where I am going with this).
Tip 3 Slowing the Rhythm of Bullies in Medicine
This next tip is especially effective if the doctor who is bullying you is keen on having a series of communication exchanges with you, and can work especially well if it’s something like email.
To perfect this you will need to adopt a “passive-aggressive” approach. What you are trying to do is break the momentum of the bully so that they don’t get rewarded by the bully exchange and eventually get bored and move on.
When a bully comes at you in full throttle it is tempting to try to respond and defend yourself. But this actually gives the bully a response and a dopamine rush which is exactly why they are engaging in the behaviour.
So rather than fight back directly. Offer to take on board the bullies comments (criticisms) and do some research or some thinking, and indicate you will get back to them. And then take your time. Chances are they won’t follow up.
If its an aggressive email. Park it and respond at another time. Chances are there are a number of issues that need responding to in the email. Just pick the lease controversial one and respond to it. Ignore the others and wait to see how the bully responds.
Tip 4 Hide In Plain Sight From Bullies in Medicine
We obviously do have to turn up to work, do our job and associate with those doctor bullies. But bullies often only notice you when they believe you’ve done something wrong or offensive. You might find it easier to “be there” but not being noticeable.
How does this work? Try being boring. Do consistent work but not good work (at least not good work that is noticed by the bully). Be quiet when others are talking in the presence of the bully. Let them be noticed not you. Find opportunities to be more engaged in other things, such as lingering over your breaks or taking a bit longer to perform that cannula that needs to be done. Anything that has you there but in the background.
For those of you who like wearing crazy socks to work (and I’m certainly a fan of crazy socks) perhaps this rotation is the time to get the beige ones out of the bottom of the pile instead.
Tip 5 Find a Human Shield For Bullies in Medicine
In Medicine, there is often several layers of hierarchy. You may for example, as a resident, find that your bully is a burnt-out senior consultant but that there are sympathetic junior consultants or specialty trainees willing to help act as a buffer or barrier for you.
Treat these people kindly (the buffers not the bullies). Not only do we obviously need more of them in Medicine. But you will also find that they can help you more if you can minimise the attention you might draw from the bully by not only doing your job well but supporting the doctor buffering you in their job.
Tip 6 Form a Team Against Bullies in Medicine
As an alternative to finding a human shield, you may be able to collaborate with your peers to alternate your exposure to bullies and assholes in the workplace. Taking it, in turn, to be in the firing line and supporting and debriefing each other as you go.
Perhaps you can make a compact with your colleague to never leave each other alone with your bully.
Tip 7 Safe Zones For Bullies in Medicine
The ultimate safe zone for trainee doctors to shield them from a senior bully colleague is the resident doctors’ lounge. A surprising amount of work can be done from most lounges these days with the aid of IT – checking results, calling for consults, and completing discharge summaries for example.
Psychologically you also know that you are safe for the time that you are in the lounge and of course you often have the support of your colleagues available.
Want a more immediate safe zone? Try the bathroom. If the bully is in full throttle and you are feeling the tears start to well up a quick dart to the bathroom could be the fix to calm your feelings and restore your resolve.
Tip 8 Early Warning Systems
Many bullies have good and not so good days. Having systems in place to prepare the team for a bully on a bad day can be helpful so that people can prepare, leave or hide, hide in plain sight or group together.
-

How to Make a Good Resume in 2020. Top 3 Errors And How to Fix.
I’ve been reflecting back on the thousands of resumes and CVs I’ve reviewed this past year. I’ve been wanting to make a video and post about this topic for some time.
It came to me one morning. I need to give you the three key tips, the three key areas where I see so many people make mistakes, which get in the way of having an effective good, great, even winning CV or resume. So what would be better than to provide you those three best tips for your Resume in 2020? Those tips are 1. Make your name the hero of the document, 2. Don’t use a photograph and finally, the most important one 3. Include a targeted personal profile or executive summary of your career at the top of your resume.
Let’s dive deeper into the reasons why these are the top 3 tips.
6 to 8 seconds to Review a Resume.
So the thing about resumes and CVS is, if you know much about them, then you know that it only takes a recruiter about six, seven or eight seconds to review a resume for the first time. This 6 to 8 seconds is all the time that that recruiter needs to make some sort of decision as to whether they want to talk to you or get you in for an interview.
So it is critical therefore that you focus a lot of your effort on the front page or the first page of your resume. Your resume’s sole job really is to get you that conversation with the recruiter or employer.
Tip 1. Make Your Name the Hero Of Your Resume.
Far too often do I see people putting non-essential words at the top of their resume, like “curriculum vitae” or “resume”. When we actually already know what this document is. So the first tip for maximizing your front page is to get rid of those words and any other erroneous text and just put your name in the biggest, boldest, largest font size letters you can at the top of the page.
Because your name is the “hero” of this document. You’re trying to sell yourself to the employer and the one thing you want them to do is to remember your name.
Tip 2. Get Rid Of That Photo.
Which leads me to the second key point. Think carefully about whether you need a photo on your resume.
Each and every year candidates ask me “should I be including a photo on my resume this year?” My advice this year is the same as before. Don’t include a photo, particularly if you are applying for a job in the professional realm.
Photos are seen as ostentatious and over the top. And the other problem with including a photo on your resume that you don’t know about is if they’ve never seen you before, the recruiter begins to make up all sorts of ideas about you in their mind based on your photo and the recruiter’s unconscious biases, rather than the contents of your CV or resume. And they are spending three or four seconds looking at that photo when they should be spending those three or four seconds out of a total of six to eight seconds reviewing other parts of your resume.
Tip 3. Incorporate An Executive Summary In Your Resume.
My third key point and the thing I see missing so often or poorly executed on CVs or resumes is what some might call the “personal profile” or “career summary”. But what I now like to call the “executive summary”. The bit that sits at the top of your resume right under your name, that takes up about a third or half of the front page that tells your story about who you are, what your career is about, and what you can offer to the employer.
The problem I see is this executive summary is either missing or that candidates are putting bullet points with responsibilities and things that they’ve done in the past that are of no real interest to the employer.
So make sure you tailor that and talk about the sort of knowledge and skills and capabilities that you can bring to the job.
But also think about what can you offer to this employer.
- What do they need?
- Can you offer new leads or new business?
- Can you offer to improve processes and reduce costs?
- Or can you actually create new value for this employer?
Write all that down and put it at the top of your resume.
Hi, I’m Dr. Anthony Llewellyn, otherwise known as the Career Doctor. If you are new to this blog, I make posts and videos on YouTube about the job application process. I am a real medical doctor who knows far too much about the recruitment process. If you want to check out some of my other posts then feel free to have a search around or hop on over to the Career Doctor YouTube channel by clicking on the video attached to this post.
Related Questions
Question. Do You Have Any Extended Information About CVs Or Resumes?
I certainly do. Check out this post or the related posts below.Question. Can You Tell Me More About the Executive Summary Or Career Goal Statement?
Again. We got that covered in this post.Question. I’m Really Struggling With My CV Or Resume. Can You Help Me?
Answer. Whilst the main purpose of this post is to provide everyone with some free information about how they can empower themselves to do better in the recruitment process I do offer a range of options to get more detailed help with your CV or resume. Just look under Services in the Header or pop over to here. -
Interview Failure. How To Not Suck At Job Interviews: 6 Success Tips
Have you ever had an interview failure before? Did you really suck in your interview! Well, this post is about how not to suck in the job interview. As an Executive and Career Coach, I have helped many candidates prepare for job interviews as well as sat in on quite a few (both sides of the table) myself. So I wanted to share with you some tips for avoiding an #epicfail in your next job interview.
What’s the best way to avoid interview failure and sucking in the job interview? Well, there are shortcuts and hacks of course. But like everything that is important in life. The number one way to avoid failure and succeed in your next job interview is ensuring that you have put in sufficient practice and preparation.
The rest of this post will be dedicated to exploring this in more detail.
Awkward Handshakes and Interview Failure.

First, off the rank, let’s talk about how to enter their job interview room and not suck in the first few minutes. One of the best ways to suck in the first few crucial minutes of the interview is to do something awkward when you enter the room. The most common trap here is the handshake.
No one wants to shake hands with a limp-wristed interview candidate. Or even worse, see someone stumbling over a desk or a chair to try and extend their hand knocking over a jug of water. That’s a really great way to get off to a bad start. You’re going to be nervous from the get-go and the panel members are going to think that you lack confidence.
So how could we not suck at that moment? Well, my first tip here is do you really need to shake their hand in the interview? Often it’s best to take the lead of the chair of the interview panel, and the interview panel members themselves. If they don’t offer a hand. Maybe don’t offer yours. Particularly if they are set up behind the big desk or it means that you are going to have to shake more than five or six hands and a big panel interview.
But if you are planning to go in with a power shake or really good handshake, why not practice that beforehand? If you’re one of those people who’s not used to shaking hands in social situations, and you’re planning on shaking hands in the interview, then incorporate this into your practice.
Not Having An Example
The second great way you suck in an interview is to not have a good example when you’re asked for it.
In most interviews for jobs these days, there’s going to be at least one question where they say, can you tell me about a time when you did…And then it’s going to be over to you.
What the panel is looking for are areas and examples of your past work or possibly even something in your education or even outside of education and work, where you can show that you’ve risen to that sort of challenge in the past before.
Now it’s extremely awkward if you have not got an example of prepared and there is a big long pause and silence while you try to think of something.
How can you know what sort of examples you need to prepare for the interview? Well if you actually go and read through the job description, you’ll find some selection criteria which give you a lot of information about the sort of examples of past work that they may want to hear from you. These would generally be about things like meeting success targets or in a team resolving conflict, and using communication skills. It depends on what the selection criteria are for the job, but if you read through those selection criteria, you can then think about your own career, your own work, your life, your academic success. And you can then think about the sort of examples that might be needed in the interview and be prepared for the day.
Gender Stereotypes

The next sure-fire way to suck at an interview is to fall for Gender stereotypes.
What do I mean about gender stereotypes? These days, most interview panels are normally comprised of both male and female members of the existing team. And they may throw a question to you, which is a hypothetical situation about working in a team and you start referring to a certain team member as she or him. But they actually haven’t given you that information.
So a classic example is inside the world of medicine where they might ask you about resolving a conflict between yourself as a doctor and a member of the nursing staff. And you start referring to that member of the nursing staff as she or her or a lady. That’s a sure-fire way of putting yourself out of alignment with any member of the panel who’s got any appreciation for gender diversity in the workplace.
So the solution here is to avoid referring to people as she and he based on stereotypes.
Performing in a job interview is a skill. But the problem with the job interview as a skill is that it is only a skill that you very rarely occasionally use and the rest of the time it’s meaningless.
Dr Anthony Llewellyn | aka The Career DoctorTalking Too Much
The next great way to suck at a job interview is actually talking too much.
What do I mean by talking too much?
In interviews, you can talk for too long in terms of your answers. You can normally tell this because you find yourself rambling on rather than being succinct and giving an organized response. Or, you can talk too much about yourself.
When you talk too long and you talk about yourself, that means that you are not talking about the actual job you’re applying for, the organization that you want to join, the interviewers themselves, and the team that you are intending to join. You are also not talking about the teams that you’ve worked within the past and the connections you might have to other people that might be helpful in the role.
This is all important stuff as it sells you to the panel. Far too often I hear people talking about themselves in “I terms” rather than “We terms” in relation to the successes they’ve had in their career
You see the panel may be looking for someone brilliant, but they also don’t want someone who’s going to dominate them. They want someone who can come in and brilliantly contribute to the hardworking and high performance of the existing team.
Silly Questions
The next way to suck at the job interview is to ask a silly question.
At the end of each interview there’s usually a time where the panel says something like:
“Those are all the official questions we have for you, but do you have any questions for the panel?”
How often have we managed to completely unravel a really good interview process by asking a silly, or stupid, or dumb question at the end of the interview?
Examples of silly questions are questions that show you really haven’t done your basic research. Such as what are the rosters for the job, or where will I exactly be working, or who will I be reporting to? Or questions that might give the impression that it’s not really the job you are interested in, but something else. Like questions about salary.
There are a number of ways of correcting this problem and avoiding sucking right at the end of the interview. One is to think about whether you really need to ask a question at all.
You can often just answer that last question by saying something like. “No thanks. I’ve had enough opportunities to ask questions already. Thank you very much for the opportunity”.
If you are really intending on asking a question then do your research and prepare a question that will dazzle them or wow them.
At the end of each interview there’s usually a time where the panel says something like: “Those are all the official questions we havefor you, but do you have any questions for the panel?” How often have we managed to completely unravel a really good interview process by asking a silly, or stupid or dumb question at the end of the interview?
Dr Anthony Llewellyn | aka the Career DoctorCan You Really Wing It?

Can you tell what all these points are leading up to?
If you have had a bad interview performance before, you’ve probably thought of a few reasons why it went wrong. It might’ve been that it was a high-pressure environment and you just got stressed. It might just be that you felt you didn’t “click with the interview panel”. It might be that they asked you all the wrong questions. Or maybe you just had a bad day.
What do all these reasons or excuses have in common?
They all reflect the fact that you probably didn’t prepare and practice for the interview.
Performing in a job interview is a skill. But the problem with the job interview as a skill is that it is only a skill that you very rarely occasionally use and the rest of the time it’s meaningless.
And the problem with skills that we don’t use very often is that they degrade quite quickly. We’re not regularly practicing our interview performance. So without regular practice and preparation in the lead-up to your interview, your interview performance is likely to suck.
So the number one tip for not sucking in the job interview is to spend the time to practice and prepare for your job interview.
Related Questions.
Question. Are There Things I Should Prepare Prior to the Interview?
Answer. There are a number of things you should try to prepare prior to the interview. These range from doing your job research, to researching the panel members, as well as more practical things like putting together a portfolio of your work, making sure you have an appropriate outfit, and working out how you will travel to the interview. We have summed up a few of the questions you should ask yourself in this article.
Question. If I Think I May Need Some Coaching For the Interview. What Should I Consider?
Coaching is a really excellent way to maximize your interview skills practice in a short period of time. A good coach will not hold you accountable for your practice schedule but also help make improvements to your technique and interview responses. However, not all coaches are the same and a general rule of thumb is you probably pay for what you get. We have summarised some of the considerations in this article.
-

Stop Asking Weird and Dumb Interview Questions. Ask These 5 Instead.
As a means for helping other doctors, at AdvanceMed we collect an open bank of real interview questions. These are questions that have been asked in a formal doctor interview process. Our community members regularly submit questions to this bank (thanks heaps by the way!). Not infrequently the questions that come through raise an eyebrow for me and I do wonder whether we are in fact providing a service to anonymously “out” weird, stupid and dumb interview questions and by proxy those that come up with them.
Here’s a recent example from a Pathology trainee interview:
So what exactly is wrong with this type of question and what makes it a “dumb” interview question? Whilst there is no issue with coming up with a challenging question for the job interview. The question does still have to make sense and allow candidates to provide an answer that helps you to judge them by the selection criteria that you have set out.
Context Is Important.
Everything is contextual in recruitment. So a question about inviting guests to dinner might well be very relevant for say an event management position, where one of the Key Result Areas is the ability to come up with a fresh program of speakers for the event sponsor.
But the selection criteria for most medical jobs that I have seen don’t include an event management function. They generally talk about behaviours such as demonstrating good clinical knowledge and skills, good communication, good teamwork, being professional, demonstrating ongoing learning, and practicing cultural respect and safety.
Maybe at a real stretch, a question about inviting people to dinner could infer something about how one goes about forming a team. But I can think of a dozen betters ways of constructing a question that gets to that issue.
Unfortunately, sometimes the doctors who attend interview panels in medicine think that because they are intelligent and perhaps have attended a one day course in recruitment and selection that they are all of a sudden an expert in human resources and recruitment and that it’s time for a “wacky interview question to challenge the candidates.”
Perhaps they may also feel that a creative thinking type of question gives them a different perspective on the candidate? Some useful insight into their personality or communication or teamwork style. But guess what? There are actual validated psychometric employment and other psychological tests that do a much better job of this than one interview question.
Stick To The Script.
I’d encourage all doctors and other professionals involved in the candidate selection process to stick to the script. By which I mean stick with the principle that each interview question should form a relationship to at least one of the selection criteria for the job.
I say this for three main reasons:
- This principle actually makes it easier to design good questions and establish rating criteria
- The information you gain from these questions from each candidate will be far more useful to you
- Most importantly you are also avoiding getting into the tricky area of problems with discrimination and equal employment opportunity
Yes. That’s right. If you can’t prove how your selection process relates to the actual requirements of the position then you open yourself up to the possibility of candidates challenging the process as being unfair.
Good Job Interview Questions. Challenging Questions That You Should Ask.
Ok. So you have looked at the list of questions you are asking for the job and they are predictable and the same as last year. You would still like to be able to stretch the candidates a bit. What can you do?
Here are 5 questions that you can probably use in your next medical job interview. Bearing in mind that you do still need to ensure that they line up with the selection criteria.
Good Interview Question Number One.
Acknowledgements to Loud Adler for this question. This one question can tell a lot about a job candidate in medicine. Starting with whether they value outcomes and achievements in their work. It can also provide insights into how they go about accomplishing success, how they manage their time and incorporate feedback into their process, whether they get chosen to work on challenges and why, and how they work with others to marshall resources and create a common cause.
There are so many supplementary questions that can be explored off the back of this one single question.
And this question is easily related to the selection criteria of most medical jobs. For example:
- Demonstrated ability to work effectively & harmoniously in a multidisciplinary team.
- Demonstrated good organisational, time management and problem-solving skills within a complex clinical environment.
- Proven commitment to ongoing learning and professional development.
- Ability to contribute to quality improvement and / or clinical safety in the hospital.
Good Interview Question Number Two.
This is one of my current favourites. Once again it requires the candidate to dig into their career and choose an example of how they have performed. This time under difficult circumstances. If the example doesn’t seem all that difficult. Then this may imply that the candidate has not been truly tested. If the example blows you away it probably means that they are up for the challenge. But its also what they found difficult and how they handled it that matters most. For some, it might be difficulties in communicating or dealing with under-resourcing. For others, it might be difficulties with the emotional impact of work. Whatever the circumstances look for evidence of personal insight, coping strategies, advocating and escalating for help and of course, relying on one’s team.
This question is easily related to selection criteria such as:
- Demonstrated good organisational, time management and problem-solving skills within a complex clinical environment.
- Ability to work independently in a supervised environment and work in a multidisciplinary team
Good Interview Question Number Three.
Most candidates can talk the talk when it comes to using evidence in their clinical work. But it is surprising how many are stumped when asked to actually recall an example where they have used evidence to alter theirs and their team’s approach to care.
This question applies to selection criteria where you are wanting to see the demonstration of up to date clinical knowledge and practice (which is pretty much in every doctor position description), but often there is also a criterion about demonstrated commitment to learning and research. So it can address two criteria at the same time.
Good Interview Question Number Four.
A much-overlooked question is why a candidate is applying for the position. Granted in many doctor interviews its a matter of progressing from one stage of training to the next. However, as we go up the seniority ranks there tends to be less turnover. If a doctor is a genuine asset then usually their manager is trying really hard to keep them. So there needs to be a good positive reason offered in terms of things like:
- desiring more responsibility
- experiences that are not on offer in the current post
Any sign of negativity towards the current employer or service should be treated with caution. Strong candidates will be more sanguine about their current experience and less likely to say anything negative regardless of how bad the experience has been.
This question is often a better alternative to asking candidates to either “Tell Us About Yourself?” or “Tell Us Why You Are Good For the Job?” It invites a candidate to address any or all of the selection criteria. Although in Medicine, most will tend to focus on the clinical requirements first in their answer.
Good Interview Question Number Five.
The last good question is in fact not a question but a test. And the test will again depend on the position and the selection criteria.
In the majority of jobs, which includes medicine, there is normally a key task that is important for the role and which can be simulated in an interview environment. Successful demonstration of this task will normally address selection criteria around clinical capability as well as often communication skills.
The “Skills Test” is used surprisingly sparingly in medical job interviews in my experience. But often very easy to deploy and quite useful.
In a past role, I recruited doctors to fill Resident Medical Officer posts in mental health. The role required a basic ability and knowledge of mental health (we could and did teach the rest) but importantly required the doctors to have up to date medical skills.
We would give each candidate a couple of ECG readings with a scenario which demonstrated common abnormal findings. This test was remarkably discriminating and quite reassuring in terms of hiring doctors who were able to interpret basic ECGs.
Some other examples where a Skills Test may be relevant:
- Resident demonstrating how to complete a pathology form or prescription
- Surgical trainee demonstrating a knot tieing technique
- Surgical trainee consenting interview member for surgical procedure
- Radiology trainee interpreting and completing a report on a Chest X-Ray
- Psychiatry trainee watching a short video of a patient and reporting mental status findings
- Advanced Trainee being asked to give a presentation on a recent update in their field
- Consultant being asked to prioritize a ward round list
Related Questions About Dumb Interview Questions.
Question. Are There Any Interview Questions That A Panel Is Not Allowed To Ask Me?
Answer. Yes. There are. These are called discriminatory or illegal questions. There are laws in Australia and most other countries to prevent panel selecting people on the basis of background, preferences or characteristics which do not relate to the ability to perform the role. We have a post about this here.
-

13 Questions to Ask Before A Job Interview
It’s been a bit of a peak period for interview coaching the last few months. One question that I find that I am often being asked at the end of an interview coaching program by a candidate is: “Is there anything I should be asking about before the interview?”. So what are the sorts of questions to ask before a job interview?
There are definitely a number of key questions you should be getting the answers to prior to going into your job interview. For some of these questions, you should seek the answer from the person coordinating the recruitment. They will include the length of the interview, the format of the interview, the names and positions of the interview panel members, and whether you need to prepare anything for the interview.
For the rest of these questions, you should be seeking the answers from yourself, and possibly your interview coach if you have one. They will include answers to what is the panel looking for, do you have any weaknesses in relation to the job, and do you have the right examples prepared for the panel.
Let’s go over this in a bit more detail. Starting with questions you can ask of the recruiter and then questions you should be answering yourself.
Questions to Ask Before a Job Interview – Question to Ask the Recruiter.
I always recommend if possible that you check in with the person coordinating the recruitment a few days ahead of time. Some recruitment coordinators are very organized in providing you with information about the process. But more often than not you can find out more by being courteous and respectful.
Remember also that this person is often also an executive assistant working with the chair of the panel. So it helps to be making a good impression. Because panel chairs often do ask about whether candidates were polite or not.
Here are some questions to ask before a job interview of the recruiter.
Confirm the Details of the Interview.
Make sure you confirm the details of your interview. Because times and locations do change and sometimes can be wrong. Especially if the interview is being done across countries and time zones. How early should you arrive? Is there any paperwork that needs to be gone through prior to the interview?
Find Out the Names of the Panel Members.
Quite often interview panels are being pulled together at the last minute. So checking a couple of days beforehand is usually the best time to be able to find out their names. I think this is one of the most important questions to be asked as it is very difficult, if not impossible, to remember the names of interviewers if you are just introduced to them during the interview.
Find out the position of each panel member and do your research on them. What is their role, profession, and what are their interests? This will help you to tailor your question responses effectively.
How Long Does the Interview Go For?
Ask about the length of the interview. How many questions will there be in total? This helps you to know how long or short your answers should be.
Is There Anything You Should Prepare for the Interview?
Some interview processes involve getting you to prepare a presentation as the first question or coming in early to review the interview questions. It’s good to know about these things as early as possible.
Is There Anything You Should Bring for the Interview?
The interview is often the time when panels will want to view your credentials and 100 points of identification and other documents like working with children checks. You should also ask if it’s ok to bring things with you to the interview. I always like to bring a portfolio of things to look at and refer to during the interview. Having the job selection criteria to look at can be particularly useful when dealing with strange questions from the panel.
How Many Candidates Are Being Interviewed?
You may think that this is a question where you are unlikely to get a response. But recruiters and interview panels can be surprisingly candid about these sorts of questions. And it helps to know your chances going in.
Its also often possible to work this out based on the length of the individual interview and the total time allotted.
If it’s a position with multiple openings try to also find out how many people the panel is wishing to hire.
If the Interview Is a Video Interview Is It Possible to Do a Test?
Many interviews are conducted these days using video. Usually, you are asked to go to a link on the web using a browser on your computer. It’s a good idea to find out details about the system being used beforehand. And if possible to test it out on your setup as well as trying to connect to another location to ensure that you have the right equipment and appropriate amount of internet bandwidth.

Questions to Ask Before a Job Interview – Questions to Ask Yourself
Arguably even more important than having full knowledge of the interview process is having full knowledge of yourself. If you put yourself through your paces before the interview you are much more likely to succeed.
So here are some questions to ask before a job interview of yourself.
Do I Understand What They Are Looking For?
It may seem obvious. But between lodging that application and doing all that preparation you may have forgotten exactly what it is the panel is looking for. Review the selection criteria that came with the job description. Check out the role description and key responsibilities. Make sure you understand what competencies they are looking for so you can talk about how your own competencies demonstrate that you are a good candidate.
Can I Paint A Compelling Picture Of Why I Am the Best Person for the Job?
Most panel interviews start with a question along the lines of “Why have you applied for the job?” or “What makes you a good candidate?.” Make sure you have an answer to this question. What are the 3 key strengths that you bring that not only meet but exceed their expectations? Use examples and storytelling to paint a compelling picture.
Have I Anticipated Any Key Weaknesses?
The panel will not just be interested in any strengths you may bring to the role. They will be interested in any areas of weakness. Overall they will be generally cautious about giving someone who has significant weaknesses the job. Even if that is balanced out by significant strengths.
So it’s important that you have honestly considered whether you are truly weak in any particular area and have a plan for addressing this weakness.
For example, if the role calls for you to conduct research as part of the position. But you haven’t done any real research. Then you need to be prepared to talk about how you have other skills that would translate to this requirement and mean that you would not necessarily be starting from scratch.
Have I Thought About What Questions They Will Ask?
If you have been doing interview practice you probably have been thinking about what questions will be asked. But be careful that you are not just practising old questions that are based on outdated selection criteria.
If you have not done any preparation at this point you should at least be going through the position description and in particular the selection criteria and coming up with at least one question for each of these.
Have I Talked to Current Incumbents?
A commonly overlooked but easy thing to do in your preparation is to talk to actual people who are doing the actual job that you are going for. These people can give you all sorts of insights into the key challenges of the role and phrases such as:
“Well, when I was talking to one of the current doctors working in the role they mentioned some key things to watch out for in the first month were…”
Will go a long way with the panel.
Current incumbents can often also give you vital insights into the selection process.
Do I Know What Sort of Questions I Need to Ask?
Perhaps the final thing to think about is whether you have any questions about the job that needs answering. There is normally a period at the end of the interview when the official questions have been asked where you have a chance to ask your own questions.
It’s important that you don’t blow your interview by asking a question to which you have already been given the answer or which doesn’t show that you have put in your research.
On the other hand, asking a really insightful question can finish off the process on a high. It’s best to have prepared these questions beforehand rather than just winging it on the day.
Related Questions.
Question. Is There A Good Approach to the Final Interview Question.
Answer. Yes, there is. This is a common “question” that I get asked about. But it depends on your individual circumstances. In many situations, it’s actually OK not to ask a question. Particularly if you don’t have a good one. Here’s a video to help you out.
Question. When Do My Referees Normally Get Interviewed?
Answer. This very much depends on how many candidates are being interviewed and also whether there is some form of automated referee checking system. If there are large numbers of candidates. Then the selection committee will normally wait till after the interview to check referees. They will generally start with referees for preferred candidates. So if your referees are being interviewed at this point it’s a pretty good sign.
-

Common Questions (and Answers) About AMC Standard Pathway
Over the last year, I have been pleasantly surprised by the interest of doctors all over the world in some of the explanations that I have been providing both here on the blog as well as on my Career Doctor YouTube channel about the processes for working as a doctor in Australia. There have been a lot of questions and comments seeking further understanding about the Standard Pathway Process. So here is a list of common questions and answers to help you out.
What is the Standard Pathway Process?
The Standard Pathway is a process whereby doctors who have medical degrees from outside of Australia can apply to have their capability as a doctor evaluated in order to work in Medicine in Australia. The process is intended to ensure that doctors are competent to the level of Australian doctors at the point at which they graduate from medical school and go onto successfully complete a provisional intern year.
Which Doctors Should Apply for the Standard Pathway?
The Pathway applies to international doctors who do not have specialist qualifications and who are not from one of the “competent authority” countries. So the majority of international doctors seeking general registration do apply for this pathway.
What Are the Competent Authority Countries?
The medical regulatory system in Australia recognizes 4 other countries as having medical training systems that are equivalent in terms of outcomes to Australia. The countries are the United Kingdom, the United States of America, Canada and the Republic of Ireland. Doctors from New Zealand are also recognized as having identical outcomes in their medical degree as the Australian Medical Council also accredits New Zealand medical schools.
This means that if you graduated in medicine from one of these countries you have a more streamlined pathway available for being able to work as a doctor in Australia.
In addition, some international doctors who have been through the process of gaining registration in a competent authority country will also be able to apply via this competent authority pathway. For e.g. if you have successfully completed the PLAB.
What Are the Australian Medical Council Examinations?
According to the Australian Medical Council
The AMC examinations are set at the level of attainment of medical knowledge, clinical skills and attitudes required of newly qualified graduates of Australian medical schools who are about to begin intern training. They consist of a computer adaptive test (CAT) multiple-choice question (MCQ) examination and a clinical examination:
- The AMC CAT MCQ Examination tests knowledge of the principles and practice of medicine in the fields of general practice, internal medicine, paediatrics, psychiatry, surgery, and obstetrics and gynaecology. It focuses on essential medical knowledge involving understanding of the disease process; clinical examination and diagnosis; and investigation, therapy and management.
- The AMC Clinical Examination assesses clinical skills in medicine, surgery, obstetrics, gynaecology, paediatrics and psychiatry. It also assesses ability to communicate with patients, their families and other health workers.
So an important thing to note here is that the AMC Exams are clinical exams and do not involve being tested around matters of basic science.
When Can I Sit the AMC Examinations?
You can sit for the AMC Examinations any time after you graduate from your medical school. All that is needed to sit is proof of a primary medical degree.
You must sit and pass the first AMC Exam. The MCQ test. Prior to being able to sit for the Clinical Examination.
Do I Need to Sit An English Test to Sit the AMC Examinations?
Surprisingly the answer to this question is no. You won’t need an IELTS test or one of the other 3 acceptable tests in order to sit the examination. However, you will likely need one in order to apply for a job and become registered. See below.
How Often Can I Sit the AMC Examinations?
You can sit as many times as you wish to. But you can only be preparing for and registered to sit one particular exam at a time. Bear in mind the exams are expensive.
Is There An Age Limit For Sitting AMC Exams.
No. You can sit them at whatever age.
How Long is my Exam Result Valid For?
Once you pass an AMC exam this result remains valid for life.
Is There a Time Limit for Sitting the AMC 2 Exam?
No. There is no time limit by which you may sit this exam.
How Much Does It Cost to Sit the AMC Exams?
The AMC Exams are quite expensive. The MCQ exam costs $3,124AUD per sitting and the Clinical exam costs $3,991AUD for an in person sitting and $4,391AUD for an online. These costs are generally more expensive than most College training exams in Australia. There are also other fees that you will have to pay, for example, to establish a portfolio with the AMC, to get your certificate or reissue results.

c/- AMC 2024
How Hard Are the AMC Exams?
In essence pretty hard. The MCQ exam is relatively ok with around about a 60% pass rate per sitting. The Clinical Examination is notoriously difficult with a pass rate of around 28%. See this post for a more in-depth explanation.
When Is the Best Time to Sit the AMC Exams?
The AMC Exams run constantly throughout the year with a bit of a break over the Australian summer period. There is no best time to sit from this perspective.
As the exams are a test of your medical knowledge and abilities at the end of medical school it is generally considered that it gets harder to sit and pass these exams the longer it has been since you yourself finished medical school. So its best to sit as soon as possible. Many doctors will sit the MCQ whilst completing their own internship year in their own country.
Is There a Waiting List for the AMC Exams?
According to the AMC there is no wait list for the exams and no need for a wait list as they are able to offer enough examination spots to satisfy demand. This is achieved by running a number of MCQ exams both in Australia and across the world as well as having increased the number of clinical examination spots available.
Whilst it may be true now that there is no wait list there have certainly been concerns in the past particularly in relation to waiting significant amounts of time (18 months or more) for the Clinical examination.
The process itself also imposes a waiting period. Because once you have applied for and selected an examination date you cannot apply for another exam date. And you have to await the results of your MCQ exam before either applying to do it again or applying for the Clinical exam.
What’s the Best Way to Prepare for the AMC Exams?
In the AMC exams you compete against a standard. Not other candidates. So most doctors who have been successful in the AMC exams will tell you that one of the best ways to prepare is to form a small study group.
Generally, most candidates prepare by using examples of past questions. You can purchase some official questions from the AMC. But there are also a number of other MCQ questions and Clinical stations floating digitally around the internet as many AMC candidates do attempt to recall questions after their exam.
Given the expense of the exams themselves, it may be difficult to afford to pay for additional resources such as textbooks and online and face to face courses. Most international doctors do recommend purchasing a copy of Professor Murtagh’s book on General Practice as this covers a lot of the Australian specific knowledge for both the MCQ and Clinical. There are also a number of online tutoring and courses available as well as face to face courses and opportunities to undertake observerships if you are able to afford these.
Follow the affiliate link below to purchase your copy of Murtagh’s General Practice.
Can the USMLE or PLAB Substitute For the AMC Exams?
Yes. But only if you complete all the steps required and in the case of the PLAB undertake at least 12 months supervised placement in the UK or in the case of the USMLE undertake at least 24 months in an accredited residency program. Otherwise, these exams are of no use and you have to sit all of the AMC Exams.
Are There Other Alternatives to Sitting the AMC Exams?
Yes. If you are from a Competent Authority Country you can apply via this pathway. If you are a specialist you can apply for the specialist pathway.
If you are fortunate to be employed at one of the 1o places that are accredited for the Work Place Based Assessment Program by the AMC then you will also most likely have the option of completing a WBA program which is an alternative to the Clinical Component of the AMC exam with a much higher pass rate and lower cost for applicants.
I Need to Complete An Internship. How Can I Obtain An Internship in Australia?
You have probably read something on facebook or the Medical Board website itself telling you that you need to complete an internship to be able to be registered. In most cases, you probably do not need to complete an internship. As you will have done something similar in your own country. In general, the Medical Board wishes to see evidence that you have been granted a full license or general registration to practice in your own country. In some cases, this may require passing an internship or similar during medical school. In others, it may mean completing a provisional year after graduating.
If you have not done any of these things so far. Then you do still need to complete an internship. But you are much better off completing this in another country. As the chances of being able to actually gain an internship position in Australia are extremely small.
Do I Need to Sit an English Test?
Most likely the answer to this question is yes. However, you may have some options to be exempt from this requirement if you can prove for example that all of your high schooling was in English.
How Well Do I Need to Do In the English Test?
There are minimum requirements for the various English Language Standard tests that you can do. For a fuller explanation see here. As an example to be able to gain registration if you sit the IELTS you need 7 or above in all four domains of this test.
Many doctors think that achieving the minimum requirement in the English test is all that is needed. However, the minimum requirements often correlate with being less than sufficient in English in the eyes of the employer and can often mean that you are rejected for an interview in the first place or find out that your English language skills were the main reason the interview panel felt you were not suitable.
You should endeavour to practice and build in your Australian English as much as possible and consider taking the test again to demonstrate a better score.
When Can I Apply for a Job?
As soon as you are successful in the AMC Part 1 you can begin applying for a medical position. Most doctors recommend this strategy and not waiting until you complete the Clinical Examination. This is because it can often take a lot of time and persistence to obtain a position. The downside of this approach is that you will probably get a lot of rejections and find yourself in a big group of candidates who all just have the AMC Part 1 exam.
What Are the Best Jobs to Apply For?
What job you apply for may depend on where you are intending to head in your career, particularly if you are looking at general practice. Bear in mind however that most of the doctor jobs in Australia will not be available to you until you have obtained general registration. The most common type of job that will be available is called a resident medical officer (RMO) job. These are often advertised at times during the year when hospitals have had vacancies in their ranks. The RMO role is normally a position that is one more year advanced than the intern position. But you are generally doing the same roles as interns, i.e. acting as the most junior member on the team looking after the day to day patient issues on the ward.
A key phrase to look for in any job description which will indicate that you can apply for a position is:
“eligible for registration”
How Can I Improve My Prospects of Gaining a Job?
I’d recommend you watch this video I did with Dr Naj Soomro. In it, we highlight a number of things that can help you gain a job.
Some of the key things are:
- Having a really well put together resume
- Establishing networks to identify ad hoc job opportunities
- Being prepared to look outside of the major cities
- Preparing for job interviews
Once I Get a Job Offer. What Happens Next?
It is very important that you ask for a contract. There have been situations where international doctors have been offered a job in the past but this has been withdrawn at a later date. You are really not secure in your job until you have started working. It’s important that you are responsive during the phase between the offer and commencing as you will need to help the hospital sort out things like your registration and visa status.
Once you are up and running you should make sure that you are aware of your supervision requirements and ensuring that you are getting regular feedback on your performance and completing the reports that need to go back to the Medical Board. It’s much better to identify problems in your performance early on so you can fix these rather than letting them become a big issue and jeopardizing your sign off at the end of the 12 months of limited registration.
When Can I Apply for Training Positions?
Once you have completed the process, ie. you have your full AMC Certificate and a satisfactory 12 month’s supervised practice you will be able to apply for general registration.
Once you have general registration you will be eligible to apply for most of the specialty training schemes.
There are some exceptions to this where you also require permanent residency. For example, the Australian General Practice Training Scheme and the College of Surgeons training programs. So, if you are aiming for these you will need to consider alternatives or wait a few more years till you can obtain permanent residency.
-

5 Killer Interview Questions to Ask Employers. And When to Use Them.
Most job applications still include a panel interview process as one of the final steps in selecting candidates. As part of this panel interview process, it is almost universally the custom to ask candidates at the end of their interview if they have any questions of their own. I am often asked by my coaching clients how best to respond in this situation. What are the best interview questions to ask employers? There is a myriad of approaches but here are 5 of my favourites.
In relation to the question about what question or questions, you should ask. The first point is that you do not actually need to ask a question. You can politely thank the panel for their time and indicate that all your questions have been answered already. You can also choose to use this opening as an opportunity to improve on one of your answers or talk about a strength that has not come out in the interview.
In terms of actual questions. If you haven’t been told already then it is often a good idea to ask a question about when the decision of the selection process will be made. Or you can ask a “future-focused” question, such as how will my performance be measured. Or you can actually ask the panel for some feedback about your interview performance.
Let’s go ahead and explore these 5 approaches in more detail. Including giving some examples of where each works best.
As a bonus. At the end of this article, I will also tell you about the best interview question I ever heard from a candidate.
You Don’t Always Need to Ask a Question.
Many candidates are of the opinion that they should have a good question prepared to ask at the end of the interview process in order to impress the panel further. Clearly part of the point of the interview is for you to impress the panel. But this needs to be done with authenticity. So it’s best to avoid trying to “contrive” a question to ask and remember that it’s your time and your interview.
If as part of your research you haven’t come up with a question worth asking, then, in my opinion, you are better off investing your time in other ways of preparing for the interview (such as practising panel questions). Rather than agonizing over developing a truly insightful question.
It’s absolutely OK to not ask a question at the end of the interview process. But it’s important that you handle this part of the discussion well. Most importantly you need to make it clear why you don’t have any questions.
Its perfectly okay not to have interview questions to ask employers. So long as you had done your research already.
The ideal situation for not asking a question is one where you have had plenty of opportunities to ask questions already.
For most of the job clients that I work with this tends to happen in relation to batch recruitment events. Such as the annual medical recruitment process where each year a number of doctors are given the opportunity to apply for higher-level training positions.
In these situations, there is usually a lot of time to prepare for the interview. As well as information provided via websites, one to one contact and information sessions.
Another scenario where this often occurs is for senior medical practitioner appointments, where often you have the chance to have an informal discussion with the chair of the panel prior to putting in your application.
A typical approach, therefore, would be something like:
Thanks. I don’t have any crucial questions at this stage of the process. The information you have provided me already via the [applicant package/information session/phone call…] was really useful. I’d like to thank you for the opprunity and look forward to hearing about the outcome of the process.
Suggested words if you don’t want to ask a question*As an adjunct, many of the panel members that I talk to about this. And I talk to many. Are of the opinion that it is best not to ask a question if you don’t have a good one. See the end of this blog post for examples of questions you should not ask.
You Can Make a Statement. Rather Than Ask a Question.
Remember. It’s Your Interview. The time at the end of an interview is your last chance with the panel. And in many cases, they are probably running a bit over time and seeing this as more of a polite process rather than expecting you to engage in a long discussion with them.
That being said. You don’t want to leave the room if you feel that anything you have said so far may have reflected badly upon you. OR that there is something that you have not said, which needs to be said.
So. In both of these cases, what I recommend is rather than use this time to ask a question. Use it to address these issues.
So, for example, if you felt you missed out on something important in one of your question responses. You may say something like:
Thanks. I don’t have a question. However, if its ok, I would just like to go back to the second question and add to my answer that I would of course also place oxygen on the patient.
Example of correcting an error in your interview.Or. If you haven’t made an error. But the panel hasn’t given you an opportunity to talk about your strengths. You can say something like this:
Thanks for the opportunity. I don’t have a question per se. However, I just wanted to highlight a couple of additional items on my CV in reference to my managerial skills. I know from the selection criteria that you are looking for abilities in this area. But we didn’t get to touch on these and I think they will be helpful for you in considering my application.
Example of using the time to highlight more strengths.Ask When the Decision Will Be Made.
It may not be immediately obvious. But for many selection processes, the outcome may not be clear. A good safe question to ask (politely) therefore is when will the decision be made?
Obviously don’t do this if you have already been told. Which may mean checking back through your emails first. And also watch out as sometimes the chair of the panel covers this at the start of the interview or often more frequently just at the end.
Finding out this information can serve a useful purpose.
Firstly, it gives you an opportunity to time your thank you email. So, if the answer to the question is in 5 days time, send a quick follow up email 3 days later. Don’t ask about the result. Just thank them for the opportunity. Its just a simple reminder that you are an interested candidate. And it may make the difference.
Secondly, it may also give you a hint as to whether your referees have been contacted already or (more likely) will be contacted and via which mechanism. This also then gives you time to follow up with your referees. You can let them know what sort of questions the panel asked and (re)brief them on your strong points.
Ask For Some Feedback.
A significant proportion of the clients that I work with have had an unsuccessful interview in the past. These problems have generally been compounded by the fact that when they have gone back to ask for feedback. The feedback that they have been provided (if any) has been largely unhelpful.
This is not surprising. Interview panels are not really thinking about providing feedback to unsuccessful candidates. They are thinking about how to choose the successful ones. They often see a number of candidates in one session. So, unless something is written down specifically, it is actually hard to recall the specifics. In addition, panels are also often wary about what type of feedback is provided so as not to lead to the risk of the selection outcome being challenged.
There is however one good opportunity to get some useful feedback about your interview performance. And that is at the end of the interview itself. When your performance is fresh in the mind of the interviewers.
The benefit of asking for feedback at the actual interview is two-fold:
- You get the opportunity to get some real and authentic feedback that can help you in the future
- You show the panel that you are not afraid to ask for feedback in a high-stakes situation, which should translate in the mind of the panel to perceiving you as someone who will take on board feedback when offered
So to ask for feedback you would say something like this:
Yes. I understand that you can’t tell me the results of the interview at this point. But I was wondering if you would be able to give me some feedback on my interview performance? It may help me to improve for next time. Perhaps there was a particular question I could have done better on.
Example of how to ask for feedback at the end of the interview.Please note in the above example I have suggested you ask for feedback on something you could have done better on. This is generally better than asking for feedback on something you did well. If you give the panel the opportunity to highlight an area of strength they will probably do that to avoid being too confronting. However, what you really want is something you can improve on.
Ask a Future-Oriented Question.
More often than not, this is my favourite last question approach. However, I would generally only use it if you feel that the interview has gone well.
The idea is to leave the panel thinking about you as a member of their team. If they are thinking seriously about what it would be like to have you on the team then you are very much in the running to get the position.
A standard approach here would be to ask the panel to give you some insight into the first few months on the job. So a question like:
Would you be able to describe to me what sort of outcomes you would be looking to see from me in the first 6 months and how I would know I was successful?
Example of asking a future oriented question.Can be a really powerful question on a number of levels.
Firstly, it gets the panel thinking about your first 6 months on the job.
Secondly, it gives the panel the message that you want to succeed and are interested in measuring your success.
Thirdly, it also provides you as the job candidate with some vital information about the team that you may be about to join. In that, if they can give a thoughtful answer to this question. They are probably a team worth joining. And if they haven’t really considered this question. You may want to rethink whether you want to work for them.
The Best Candidate Interview Question I Ever Heard.
I promised at the start of this post that I would share with you the best ever response to the final question that I heard (obviously as part of an interview panel). Whilst I have been on many medical interview panels in my time. The actual best question came from an interview I was involved in for a health manager role. And it wasn’t so much the question that I remember but also the approach to it.
We were looking for someone with strong project management skills and the ability to work with the existing team, which had a reputation for being disruptive in a good way, but this reputation did not suit every candidate. On our panel was me as the chair, the team member who would be the new hire’s manager and a job expert, who would be the new hire’s colleague.
The person we were interviewing had impressive credentials and was equally impressive in her responses to our questions. What sealed it for me, however, was her insightful question at the end.
She chose to not look at me nor the potential new manager. But directly looked at the job expert (team member) on the panel and asked:
What do you like about working here?
Now. Others may be not so impressed by this question. But as someone who does highly value culture in teams. I was blown away by the fact that the candidate chose to dig into the team culture and bypass the management layers to get a more authentic response.
Interestingly it figures as the first question on this list of suggested questions to ask at the end.
Footnote. We offered this person the job. But unfortunately, she had been interviewing with other organisations and we were pipped at the post.
Related Questions:
Question. Are There Any Particular Questions I Should Not Ask At the End of the Interview?
Answer. Yes. There are a number of areas you should steer clear of. They basically involve any question that might cause the panel to doubt your passion and interest for the work versus the actual job.
So. Questions about salary levels or arrangements. Concerns about overtime or secondments. Or requests to not work with certain teams. Are best left to another stage of the process.
Question. Is There Anything Else I Should Consider Doing at the End of the Interview?
Answer. You should always check with the chair of the panel if they are finished with you for the time being. Sometimes the person administering the interview process may want you to sign some forms and/or show them some documents, like identification or working with children’s checks.
If you are unfamiliar with the organisation and have not worked there before. It’s probably also a good idea to have a look around after the interview. This is helpful to you and also shows your genuine interest in the job. It’s best, however, to arrange for a tour ahead of time. Rather than just raise it as an idea at the end of your interview.
Question. Should I Shake Hands At the End of the Interview?
Answer. This is a tough one to answer emphatically. In general, it’s best to take your queue from the panel. If they offer a hand then you should shake it. Otherwise, it’s ok to just leave with a smile on your face.
-

How To Predict Interview Questions. A Sure-Fire Method With Examples.
Are you looking for an easy way to predict the types of questions you will get at your job interview? I’ve worked with lots of candidates for various jobs both inside and outside of medicine and there is a reasonably simple and straightforward method that I show these clients which can help you to predict interview questions for the majority of questions that you will normally be asked during the interview. And this method also set you up for any unexpected “curveball” type questions.
So how can you tell what sort of questions you are going to be asked during the interview? The simple answer to this is that the genesis of each interview question should come from the selection criteria that are attached to the job description. If you can identify these selection criteria then you can also identify the types of skills, strengths, evidence and examples the panel will be looking for in the interview and practise questions formatted in the various interview question styles.
Whilst, it’s never 100% possible to completely predict the actual question you may be asked. I find that this sort of analysis paired with an intensive practice regimen will pick up about 80% of the actual questions fairly closely. But it’s always possible for the interview panel to go “off-script” on occasion, especially on medical panels, where some of the panel members can view themselves as self-taught experts in the process. For these occasions, I have a couple of other methods so you can handle the more odd question comfortably as well.
For the rest of this article, I will take you through my method for identifying questions in more detail. Give you a couple of examples and then talk about a couple of more tips to have you extra prepared.
How to Predict Interview Questions Step 1. First Find the Selection Criteria.
When you know how and where to look. It’s actually pretty easy to predict most of the questions you will be asked.
So here is a typical Senior Resident Medical Officer job from the NSW Health site.
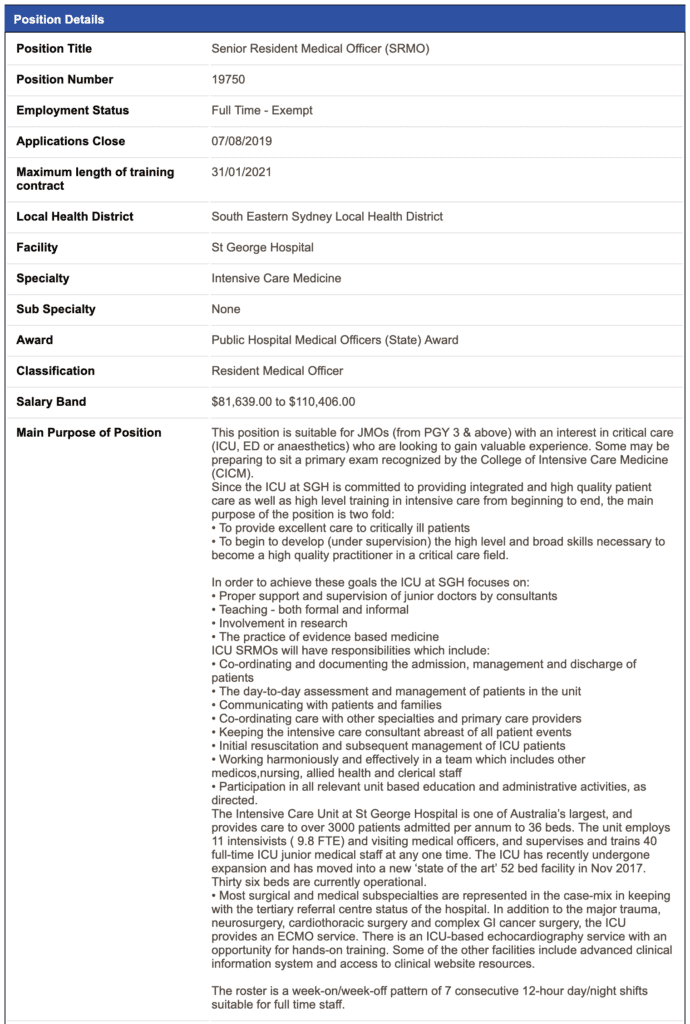
SRMO Post You can see that its for a role in Intensive Medicine. So the sort of doctor who might be applying for this role is someone in their third year of Medicine who is looking at potentially training in ICU or perhaps Anaesthesia in the future.
These jobs aren’t formally accredited for training. So they are almost 100% done as a small panel interview with perhaps 3 or 4 people on the panel.
So its obviously worth reading through the whole position description to see if it is a job that is good for you.
But once we have decided we are interested in the job. If we want to work out the sort of questions we will get asked then we need to look at the Selection Criteria. Because in most countries like Australia the common practice (and normally also the policy) is to ask questions based on the selection criteria. Here are the Selection Criteria:
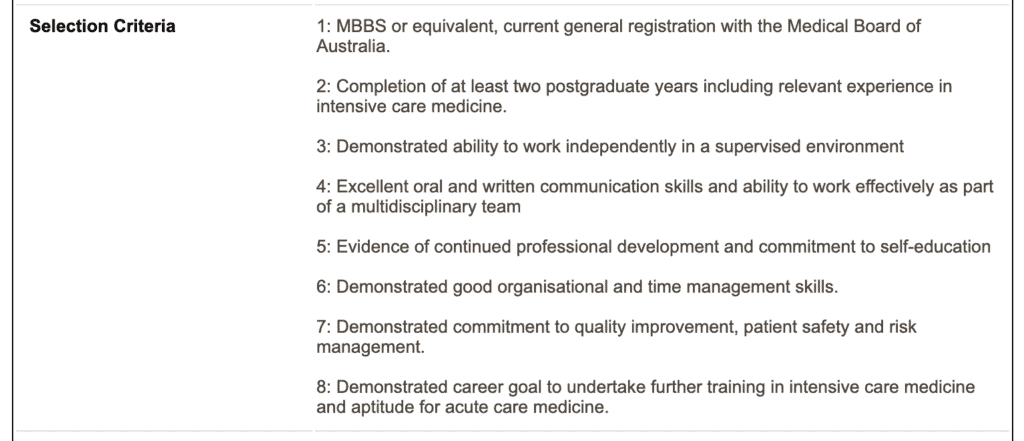
Selection Criteria In theory, you should not be asked a question which is not related to one of the selection criteria.
So for this job we have 8 selection criteria which is the maximum allowed in NSW Health. Let’s look at some of these criteria. I am going to skip over the first one which is about having a medical degree and being registered with the Medical Board. You will need to be able to prove this when you apply. So you are not going to be asked a question about this. Unless there is a specific doubt or query about the evidence you have given.
Questions About Relevant Experience
Lets look at Selection Criteria number 2.
“Completion of at least two postgraduate years including relevant experience in intensive care medicine.”
On the surface, this seems similar to the first criteria. In that, you either have this or don’t have this. But there are actually a few ways this criterion could come up as a question
AND a few ways of answering it.
The first way this criterion could come up is in what I call “The typical opening or first question.” Panels often like to kick off the interview with a question that gets the candidate to talk about themselves. So you might be asked something general like:
“Why are you a good candidate for this role?”
OR even more general like
“Why are you interested in this position?”
Or more specific and more targeted to the criteria. Like
“Can you outline how your experience makes you suitable for the position?”
If the panel was to ask this question in a behavioural format. Which they often like to.Then they might ask a question like:
“Can you give us an example of how your experience so far has prepared you for this role?”
Every Question Is An Opportunity to Highlight Your Strengths.
Now. I have just given you 4 questions that fit one selection criteria. So, you could now go off and practice all 4 questions. But actually, whilst the format of answering each of these questions will differ slightly. The content will generally remain the same.
With each and every question it’s an opportunity for you to emphasise your strengths to the panel. So in this instance, you would:
- Give an outline of your experience so far. Especially if it is more than 2 years.
- Talk about any specific experience in intensive care if you have had some.
- But also talk about related experiences and training, such as working in emergency OR doing an advanced life support course OR being given the opportunity to participate on a Medical Emergency Team
- And give the best example of a case of a patient requiring urgent or intensive care and how you contributed to that case and displayed skills and competencies relevant to intensive care.
Demonstrating the Ability to Work Independently.
Let’s look at one more of these criteria. Let’s look at number 3.
“Demonstrated ability to work independently in a supervised environment”
More often than not. The most likely way this selection criterion will be assessed is through a clinical scenario.
If you undertake any coaching with me or take my interview skills course. We talk about how the clinical scenario is both an assessment of your clinical knowledge but also an assessment of your ability to seek help and access other resources.
So, you are likely to be given a scenario where you have to have a method and approach for assessing a sick patient. But there will be a point where the panel expects that you discuss when you would seek help from more senior colleagues. And this is likely to be the more critical part of the question.
The approach to the question is to show a balance between being able to act calmly in a situation, collect information and conduct an initial assessment and then use your assessment to gain input from the senior colleague.
Once again. As always. An example. It doesn’t need to be the exact scenario but just something similar. That demonstrates how you have actually done this before in real life is EXTREMELY POWERFUL.
Some Other Tips For Being Prepared For the Interview.
Question Banks.
Another great tip for making sure you have practised the questions that you may be asked at the interview is to find out from previous candidates what sort of questions they have been asked.
You will find that if you ask around you will often be handed a bunch of “past questions”. If you get enough of these you will start to notice a bit of a pattern. That is the questions will start to repeat themselves. They may not be exactly the same. But in essence, they are the same question.
This is because medical position descriptions generally don’t change much year to year. So you can be fairly confident in using these questions to practice. And if you practice enough of them. Then you will find that you are familiar with most of the questions you get asked.
By the way, we have a page on the AdvanceMed site that lists over 500 interview questions. Categorized by various job titles. It’s worth exploring. Even if there are not many questions for your particular position. You will probably find questions under other categories are easily adapted.
Prepare an Example for Each Criterion.
My last tip is to have a good example for each of the selection criteria. This is useful. For a couple of reasons.
Firstly. You probably have had to do this anyway when you addressed the selection criteria in your application.
Secondly. Even if you are given a bit of a curveball question and you weren’t prepared for it. Having an example for each selection criteria will probably give you something to talk about that is relevant to that “curveball question”.
So that’s how you can work out the sorts of questions you may be asked at the interview.
If you are looking for even more guidance you may want to look at purchasing our book
Or check out the courses and coaching available through this site.
Related Questions.
Question. Where’s a Good Place to Find Evidence for the Selection Criteria?
Answer.
I find a good place to start is your CV. Look at each selection criteria and then go through your CV and highlight areas that meet that criteria. Ask yourself is there enough detail here? Are there quantifiable results or a good example? If not you probably want to add these into your CV for this particular job application.
Question. Why Do Interview Panels Like to Ask Behavioural Questions?
Answer.
Behavioural questions are when the panel asks you for an example from your past that demonstrates a selection criterion. This is based on some reasonable evidence from organizational psychology and human resources research that asking for an example is more predictive of future performance than an answer to a hypothetical question. Its based on the principle that past performance predicts future performance.
-

Should Colleges Be Able to Charge a Fee to Applicants?
I was recently alerted to a concerning trend in medical training in Australia which is to make trainee doctors pay for the college selection process through a cost-recovery process. With some colleges now charging over $1,000 just so a trainee can go through the process of applying for training with no guarantee of a post at the end of this.
A Situational Judgement Test (SJT) is a form of psychometric test used now in many industries to aid employers to select the best candidate for the role. Its purported benefit is that, rather than being an “off-the-shelf” test, it is specifically designed or selected to mirror the types of challenges and dilemmas an employee might be required to deal with on the job. In theory its a more direct measure of actual job related behaviour.
If an employer was to decide that they wish to use a psychometric test in a job selection process then they would normally include this in the sequence of other selection tools, generally prior to the main interview round, and organise for the potential candidates to sit this test at the employers expense.
Many of the medical colleges in Australia have made efforts of late to improve the quality of trainee selection. This includes utilising tests like the SJT. As a passionate advocate for evidence-based selection I applaud these moves. However, I was recently alerted to a concerning trend in medical training in Australia which is to make trainee doctors pay for the college selection process through a cost-recovery process. With some colleges now charging over $1,000 just so a trainee can go through the process of applying for training with no guarantee of a post at the end of this.
The Royal Australian and New Zealand College of Ophthalmologists now charges a non-refundable fee of $1200 AUD. But does not indicate in its official information what this fee is for. The Royal Australian and New Zealand College of Obstetricians and Gynaecolgists advises that “all applicants will be required to pay a non-refundable application fee in order to apply for a training position” of $570 and that “applicants shortlisted for interview will be required to pay a non-refundable interview fee” of $880. The Royal Australasian College of Surgeons applies a “processing fee” for trainee applications of $880. The Australian and New Zealand College of Anaesthetists have an application fee of $740.
But not every college charges an application fee. Some, including the Royal Australian and New Zealand College of Psychiatrists and the Royal Australian and New Zealand College of Radiologists only choose to charge a registration fee if trainees are actually selected into training.
My view is that a small application fee is perhaps reasonable in some cases, particularly high demand specialties, in order to discourage excessive and frivolous applications. But efforts to make trainee doctors pay for the actual cost of the process of selection are unwise and unfair. And particularly risk discriminating against many members of the medical community who may not be able to afford such significant fees for a host of reasons.
What About Specialist Assessments?
And the issue does not stop with the matter of trainee doctor applications. If you are an international medical graduate and specialist be prepared to part with tens of thousands of dollars in some cases to go through the full specialist assessment & recognition process.
What Are The Issues?
There are a number of issues here.
First, is the need for colleges to have some form of selection into training that seeks out the best candidates, but is also transparent fair and encourages diversity.
Second, is the cost of carrying out this process which would include things like the costs of college professional staff time, the lost opportunity cost of the time spent by college Fellows involved in the selection process, the cost of developing the selection process (SJTs are not cheap to develop), as well as potentially travel and accommodation and venue hire costs, IT costs and other costs. So significant costs.
Third, is the question whether colleges should behave the same as employers in this situation or be allowed to act differently because they are not employers? Which then draws in the issue that colleges act in a legal monopoly situation in this country. In that, through their membership, they control who is permitted to provide certain services, thus making membership of a college particularly valuable.
Fourth, is the acknowledgement that costs do inevitably need to be borne by someone or something.
To the above I will also add the question. Why do some colleges choose not to apply a selection fee or cost-recover when some do?
Are Colleges Really That Different to Employers of Trainees?
I don’t buy the argument that colleges are not employers (and therefore don’t have to act like employers). Colleges still operate as businesses to fulfill the needs of their members. Colleges are in fact in the business of making Fellows. They just don’t have to deal with competition in an open market, like most other employers.
If you lived in a small rural town and the only supermarket started charging application fees to young members of the community interested in working at the supermarket. Would that be a fair and ethical situation?
Trainee doctors are generally in a better financial position than a supermarket worker and can arguably afford a moderate application fee. But relative remuneration for trainee doctors has declined of late with significant reductions in hospital over time. And I have discussed on this blog before how specialist doctors are able to make significantly more remuneration than the trainee doctors who support them.
And it is not 100% the case that a trainee doctor can afford the significant costs required to get into a training scheme and remain on it. These costs start with paying off around $50,000 of university HELP debt or perhaps servicing a loan of $250,000 if you pay up front fees. They can then include paying tens of thousands of dollars for a Masters Course or several thousands of dollars for various short courses to improve your selectability prospects with a college. Then there is whatever application or interview fee that is posed by the college. And once you are into training around 2 or 3 thousand dollars per year of training fees, plus various examination and assignment marking fees that generally add a few more thousand dollars per year to the cost.
Why Fairness and Transparency Is Not Enough
If you have been privileged enough to grow up in a middle or higher income family with financial support, free room and board, and you are working as a resident now then you are probably managing these costs okay.
But imagine if you are the first person from your family and community ever to do medicine. Imagine if you and your family had to scrap and sacrifice to get you through medical school. Imagine if you were having to work more than part-time just to make it through medical school. You are now a resident but your debt situation, your financial security and discretionary capacity is likely to still be far worse than the example of the doctor above.
Imagine adding to this that you are a single parent doctor who needs to work part-time. Yes these doctors do exist in resident land and they are some of the most courageous doctors you will ever meet.
You can perhaps see now why just having a fair and transparent selection process with a fee of over $1000 is not OK. As it actually can serve as a real barrier to some candidates. Fairness and transparency is not enough in candidate selection as these principles on their own do not encompass the reality that not every candidate comes to the selection process on the same level footing.
The Privilege of Fellowship
The day one becomes a Fellow of a College, as I have, is truly a pivotal day. Not just in ones career but also ones life. It opens you up to all manner of freedoms and opportunities that you just don’t get if you only have general registration. Its a position of privilege that society has elected, through the activities of Colleges, to give to you and (depending on the college) a few other hundred or thousand other doctors.
Most Fellows of colleges have and continue to respect this privilege. They do this in many ways. One of these is to pay college fees to pay for college staff and resources and another is to contribute on a voluntary basis to the work of the college. Traditionally, this is how the majority of the cost of performing the activity of selection into training has been borne in colleges.
I would argue that this should for the most part remain the cases. Colleges cannot exist without trainees. Selection into training is a business cost for colleges.
As to why some colleges choose not to have an application fee. I suspect in some cases it is because these colleges strongly feel that they need more members and do not want to impose unecessary barriers.
-

Area of Need Australia. What is it? Who is eligible? How to apply.
Featured image shows the distribution of population areas according to the Modified Monash Model c/- DoctorConnect site
Post Update: I continue to get regular queries about identifying Area of Need posts in Australia. Whilst the AoN system does still exist in Australia. These days it is very rare to come across an AoN designated position for any specialty. In the majority of cases, potential employers are requiring Specialists to go through the college assessment process, otherwise known as the Specialist Assessment Pathway, first before considering them for a position. You can find out more information about the Specialist Pathway here and here.
When working with specialists from countries other than Australia one of the topics we often cover is the issue of Area of Need posts. Area of Need, which is generally abbreviated to AoN is one of a number of aspects of the Australian health care system that is difficult to understand. What is also frustrating is that apart from some notable exceptions it is also difficult to find out how to apply for an Area of Need position. I am writing this post to better inform you about AoN.
Firstly let’s answer the question of what is Area of Need and how does an Area of Need post differ from the specialist assessment pathway to specialist recognition in Australia. An Area of Need is a location where there is a demonstrated shortage of suitably qualified medical practitioners. An Area of Need post is a position that is specifically established for an international doctor to work in Australia because it has been difficult to find an Australian doctor to work in that position. Whilst historically Area of Need positions have been declared for both trainee and specialist roles. They are generally now mainly declared for specialist positions. With the exception that Area of Need roles are also often declared for IMG doctors to enter into general practice in a training capacity. Area of Need positions then vary from the specialist pathway in two main ways. Firstly, they are not always related to specialist roles. But mostly are. Secondly, they still require an assessment of the specialist IMG doctor’s potential to become a specialist in Australia through the relevant college. But as part of that assessment, the college will also consider the doctor’s suitability for the actual Area of Need position.
OK. So now you know what Area of Need is and that it is essentially an add-on option to the specialist pathway. Let’s look at a few other aspects of Area of Need that are worth knowing about, including: How are AoN positions declared? How do you find an AoN position? What are the advantages of an AoN position? And how does AoN affect the Specialist Assessment process?
How is an Area of Need Position Declared?
The authority for declaring such positions lies with the state governments of Australia (not the Commonwealth government).
Medical practitioners with limited registration for area of need are working under supervision in an area of Australia where there is a shortage of medical practitioners. They are usually registered to practise in a rural or remote location.
These practitioners have been assessed as having the necessary skills, training and experience to undertake this practice safely. The state or territory Minister for Health (or their delegate) must declare that the area in which the applicant will work is an ’area of need’.
The process can vary between jurisdictions but generally, there are two main criteria that need to be filled before an Area of Need position will be approved.
Firstly, there must be some reason for the vacancy given along with a consideration on the impact upon the community and service delivery as well as access to alternate services and options explored for delivering care in an alternative manner. The impact upon particular populations, such as rural and remote and Aboriginal and Torres Strait Islanders may also be considered.
Secondly, there must be evidence of “labour market testing”. Basically, this involves demonstrating that there have been attempts to find suitable candidates from amongst the Australian trained doctor pool but this has not been fruitful. So for example, attempts at advertising and results of previous recruitment campaigns.
Certain Doctors Cannot Work Under Area of Need.
For fairly obvious reasons doctors with general registration or specialist registration cannot apply for an Area of Need position.
New applicants who are eligible for the competent authority pathway or who already hold the AMC Certificate are also not eligible to apply for limited registration and therefore cannot apply for an Area of Need position.
Finding an Area of Need Position.
You would think with the many doctor shortages in Australia. Particularly rural and remote Australia. It would be relatively easy to find out all the Area of Need positions.
Unfortunately, no central list actually exists. This is because the states and territories are both responsible for declaring Area of Need positions as well as determining how these declarations occur. And there is no requirement for these declarations to then be listed or reported anywhere. So there is no central list. And very few of the states and territories publish a list. Even when this list is published it may be out of date.
At present only NSW Health reports what purports to be an up to date Area of Need list for both General Practice as well as other Specialties. Although I have personally found that when you enquire about some of the positions on the list there is no response or the position has been filled. Western Australia’s list is “UNDER REVIEW”. And Tasmania is only currently reporting GP posts. With Specialist posts also under review.
Northern Territory, South Australia, Queensland, ACT and Victoria all have information about Area of Need on their respective health services websites. But no list that I have been able to find.
So. What other options are there for finding an AON position?
Well. Sometimes a job may be advertised as being Area of Need. Here’s an example of a Radiologist Position in Victoria advertised on Seek as Area of Need:
But some jobs may also be advertised as seeking or being open to international doctors and you only find out that it is eligible for an Area of Need candidate when you speak to the recruiting person. This can often be the case if they are also hoping to still get a more local candidate or perhaps a specialist from a competent authority country.
AoN jobs are sometimes also posted on college websites.
Area of Need Positions Come with Advantages
Ok. So thus far. It seems like identifying an Area of Need position is becoming more difficult than its actually worth. Why would an international doctor bother trying to find one in the first place?
Well. There are a couple of key reasons why it is in fact worth the bother.
The first reason is that an Area of Need position is a real job. A job which you can apply for and hopefully be appointed to prior to having to deal with issues around registration and visas.
The effect of this is that you enter the specialist assessment process with a specific position that provides the level of supervision that you will likely be required to be given should the college approve you to undergo a specialist assessment period.
A number of IMG specialists are now going through the specialist assessment process with no guarantee of a supervised position afterwards. So they are both bearing the full financial cost of this process as well as the risk that there is no suitable job at the end of it.
In fact, some colleges, like the College of Psychiatrists will not consider you if you do not have a position offer. Probably because they do not want to be in a position of granting false hope to someone.
The second reason for obtaining an Area of Need position is that generally speaking if you have secured such a position then you have an employer who will support you through the process of applying for specialist assessment and your registration (as well as visas if you need one). This generally extends to paying for the costs of the assessment, which can be substantial. And will also extend to the costs of the college supervision if you are given the go-ahead to undertake a period of assessment.
Area of Need and the Specialist Assessment Process
One key difference between Area of Need and the Specialist Assessment process is that with AoN you start off by applying for a job. This job has been declared to be suitable for an IMG specialist and so if you are able to be successful in being offered the position it is likely that you are also a strong candidate for the specialist assessment process. Otherwise, you are unlikely to be offered the position in the first place.
Before you take up the position however you must be assessed by the relevant specialty college to determine your suitability for specialist assessment. Just like any other specialist assessment process.
The process is essentially identical. It is a dual assessment process. The college reviews your general suitability or “comparability” as well as suitability for the AoN post. You may have to fill in slightly more paperwork. There may be an additional fee. The interview questions are likely to be the same.
You can, of course, apply for other suitable jobs if you are an IMG specialist and then seek specialist assessment and this is actually a smart way to do it if you are able to.
What Specialties Require Area of Need?
Wait long enough and most specialties and subspecialties will be listed for an Area of Need position. But here are some of the more common specialties, based on reviewing the past Tasmania list and current NSW and Western Australian lists:
- General Practice
- Radiology
- Psychiatry
- Physicians (Internal Medicine Specialists)
- Various Surgeons
- Ophthalmology
- Anaesthetics
- Emergency Medicine
- Dermatology
Area of Need in General Practice
Doctors applying for registration to work in general practice must provide evidence of a minimum of three years (full-time equivalent) experience working in general practice or primary care. If a doctor has had their experience formally assessed by the Royal Australian College of General Practitioners (RACGP) or by the Australian College of Rural and Remote Medicine (ACRRM) this assessment is reviewed by the Medical Board. Otherwise, the Medical Board assesses a doctors experience as part of the application for registration. There is a minimum requirement that evidence from one of these two colleges that confirms at least three years (full-time equivalent) experience working in general practice or primary care.
Unless you are also applying for specialist assessment as a general practitioner you will also need to sit a Pre-Employment Screening Clinical Interview or PESCI.
Related Questions.
Question. How Much Does it Cost to Become a Specialist in Australia?
Answer.
It is difficult to quantify this question as each specialty differs because each specialty is handled by a separate College. As I have highlighted in this post on UK doctors moving to Australia costs for specialists migrating are certainly going to be in the tens of thousands of dollars when one takes into account the following:
- costs of both the initial college assessment as well as period of supervision
- registration costs
- visa costs
- travel, accommodation and moving costs
The good news is. As I have highlighted above. If you get the right job first the employer is likely to pick up a large part of theses costs.
Question. Is the Process of Specialist Recognition Difficult?
Answer.
Again. The answer to this depends on a range of factors. The process of becoming a specialist has arguably become a little bit easier and more streamlined in the last few years since the Medical Board has become involved in monitoring the activity of the specialist colleges and setting standards for how specialists are assessed.
In 2017, 52% of doctors were assessed as substantially comparable and 27% were as deemed as partially comparable for specialist recognition. But rates vary between the country that you trained as a specialist in and between specialties.
Its probably reasonable to say that now there is more clarity in the system and for most colleges plenty of information about the specialist assessment process most IMG specialists are probably only applying for specialist assessment now with reasonable confidence that they have the evidence to be deemed comparable.
Question. How Long Does it Take to Gain a Specialist Job in Australia?
Answer.
Many IMG specialists can search for years and not find a job. Its really hard to put a clear timeframe on how long it may take. Its reasonable to assume that it will at least take a few months. Bearing in mind that the initial job you may gain might not be quite at the specialists level. Particularly if you are only deemed as being substantially comparable.
Question. What Is A PESCI?
Answer.
International medical graduates (IMGs) applying for limited registration or provisional registration may be required by the Board to undergo a pre-employment structured clinical interview (PESCI).
A PESCI takes the form of a structured interview which can only be conducted by accredited bodies. It is an objective assessment of knowledge, skills, clinical experience and attributes to determine suitability to practise in a specific position. The PESCI consists of a structured clinical interview using scenarios.
Who Needs a PESCI?
The Board has decided that IMGs who are applying for limited or provisional registration to work in general practice are required to have a PESCI. IMGs in the specialist pathway do not require a PESCI as they are assessed by the relevant specialist medical college.
You should generally only arrange a PESCI before applying for registration if you can meet all the required registration standards. There is no point doing a PESCI if you are not going to be registered for any other reason.
At the PESCI, a panel of interviewers assesses your training, knowledge, clinical experience and attributes against the requirements of the specific position for which you are seeking registration. The PESCI process takes into consideration the supports, orientation and level of supervision that can be provided.
The PESCI uses a set of structured questions and scenarios in an interview setting which are tailored to a specific position. The report of the PESCI cannot be transferred to other positions.
The interview panel consists of a minimum of three interviewers which include at least two registered medical practitioners. One member of the panel may be a layperson, other health practitioner or registered medical practitioner. The PESCI panel members will be familiar with the clinical and professional demands of the type of position for which registration is being sought.
-

Locum Doctors Australia. How To Become One and How to Stay Current.
A recent series of articles in the Sydney Morning Herald highlighted the rising rate of medical locum doctor usage in Australia. The articles indicated that an average of 16.5% of doctors working in the NSW Health system are locum doctors. So it seems there is a trend towards locumming as either a career or a break in one’s career in Medicine. In this article, I would like to briefly cover how you can become a locum As well as address an important issue for locum doctors which is about staying current and registered as a locum doctor.
So firstly what are the basic requirements for locumming as a doctor in Australia? The key requirements are that you either have general registration and/or specialist registration. You can either locum as a Specialist (includes General Practice) in which case you need specialist registration. Or you can locum against a vacant hospital role (usually a trainee role) in which case you need general registration. By their very nature locum positions are temporary and therefore not open to doctors on other types of registration because they require a level of independent practice. So this means as a minimum you will need to be at postgraduate year 2 and have your general registration. Beyond this basic requirement, you will need to be a citizen or permanent resident, which is most locum doctors in Australia. Or possibly be on a visa which permits you to work as a locum. You will most likely need to register with at least one medical recruitment or locum agency. You will probably need to either not be currently employed as a doctor or on a break from your role. And you will likely need to consider setting up a limited company to collect payments that you make as a locum doctor.
Beyond these basic requirements, there are a number of other considerations for doctors who work as locums, which I will now go into.
Registration Requirements
As we have noted the nature of locum jobs is that they are temporary and time-limited and notwithstanding the current reporting on their usage, they are not generally seen as a permanent workforce solution. Locums are also often seen as quick and urgent solutions to filling a gap due to an unforeseen circumstance. For these reasons, it is generally not possible to set up a locum appointment for anyone who may need one of the special types of registrations available under the Medical Board of Australia where certain supervisory requirements may need to be demonstrated to be in place. In fact, often the reason a locum is being sought is that there is a lack of supervisors available. So this generally means that International Medical Graduates can generally not obtain a locum position. Although there have been some limited circumstances where it has been possible. This has generally been around deputizing services for general practice where medical recruitment agencies themselves have set up a service and essentially employ the IMG doctor.
Locum Doctors Provider Numbers
Locum positions (even ones for trainee doctors) are often advertised with a request for the locum to have a provider number. This may be just for referring purposes or for billing purposes as well. Performing locums in private practice, such as general practice is fairly impossible without a provider number as you will not be able to charge patients Medicare fees for the services you provide and the locum position will therefore not be viable.
Provider numbers can be quite confusing and complex. Part of the problem is that each provider number is generally linked to one medical practitioner and one location. Technically you need a provider number for each and every location that you provide services at or from. This can obviously be hard to predict if you are locumming. There are some solutions to this issue in relation to general practice but often what needs to occur is to fill in a form for another provider number. As it takes time for Medicare to approve this as a locum you need to be on to this issue promptly.
Other Skill and Experience Requirements
Services advertising for Specialist Locums are generally happy to accept anyone with the appropriate Fellowship (although there are some exceptions). For general locums, the amount of experience you have as a doctor will count towards how eligible you are for a locum as well as how much you will be paid. Having additional skills such as the various advanced life support training certificates or experience in paediatric emergencies will also open up the number of posts available to you as well as the rates you can collect. So, whilst you can technically locum as a PGY2 your prospects may be even better if you wait until PGY3 or PGY4.
Working as a Locum On a Visa
As mentioned above there are limited circumstances where a locum doctor may be able to work under a visa arrangement. Generally speaking, this would occur when you have general registration or specialist registration and the medical recruitment agency can obtain a visa on your behalf.
In most cases, you are probably better off working under a more secure form of employment until you are able to apply for permanent residency and then looking into locum work. This way you will not be obligated to one particular locum company.
Working With Medical Recruitment (Locum) Agencies
I’ve previously written in more detail about working with medical recruitment agencies. However, a key question about becoming a locum is whether you can work with a locum agency. This is because whilst it is possible to directly contract yourself for locum roles. Most doctors do find it easier and more productive to engage with a locum agency.
For the most part, most doctors find working with a locum agent to be a valued and essential part of the role. Someone who understands their requirements and negotiates on their behalf. But this is not always the experience. If you are not the sort of person who is good at negotiating conditions of employment you may find locum work difficult. Locum agents play a difficult role in attempting to keep the employer and doctor happy at the same time. Sometimes the conditions of the job are not as agreed to initially or sometimes you may feel pressured to take on a role that you don’t wish to do. So being able to stand up for yourself in this situation is an important consideration.
Can You Work As a Locum Whilst Employed?
If you have a permanent position with an employer, such as a hospital, it may still be possible to do the odd shift or week of locumming. But beyond this and even including this it can get difficult. Apart from the fact that you obviously need to have the time off work to do locum shifts. There is also the need to consider that you will probably be working in a situation of conflict of interest. Most employers have a process whereby full-time employees are obliged under the code of conduct to declare any additional work undertaken with the option for the employer to indicate to the doctor that they cannot undertake that additional employment if it conflicts with them completing their other duties.
Even if you work part-time it may be difficult to work part-time in a permanent position and locum as most locums are done in blocks of weeks rather than days.
So essentially whilst you may be able to do a small amount of locuming whilst employed. If you are planning on doing more than a little bit you cannot really do this whilst also employed.
Getting Paid As a Locum
There are essentially two options here and sometimes it comes down to the employer’s choice. Some employers will opt to pay you through payroll in which case they will also pay the ATO the requisite amount of tax on your behalf and should also pay superannuation on your behalf. Your Locum Agency then charges them an additional fee for placement. Others will pay you a set amount as part of an invoice you submit for the contract. This is often paid directly to the locum agency where the agency takes out its commission and then pays you out.
If there is a choice between PAYG and invoicing you can opt for either option.
As a locum, you are not going to be paid a regular fortnightly salary. So this means that you need to be prepared for being paid late, having to chase up on income every now and then and have some amount of cash in the bank to keep up all your regular payments (rent, mortgage, food, car, telephone bill etc…) in the interim.
You will also most likely need to set aside some of your income for tax purposes. Otherwise, you will get hit with a large bill come tax time and needing to take out a loan to pay it.
Some doctors find financial management a hassle. Good locum agencies will generally help you by chasing up on payments and providing your reports. But if you like a less complex set of financial circumstances then locumming is probably not for you.
Running a Company
Eventually, most doctors who locum set up a company in which to collect their earnings. There are several reasons for this. Part of which is that some health services like Queensland will not pay locums as what is called a sole trader. The other main reasons are to reduce tax obligations and protect your personal assets.
Running a company does not need to be overly complex. Most accountants will gladly help you to set up a simple company for a small fee. You do need to do some regular book-keeping and complete some additional tax forms quarterly and annually. It makes sense to set up a separate company bank out to make the book work easier.
Many doctors actually find the idea of being the Managing Director of their own company a little bit exciting. You get to pick your own company name and you can even get a logo, letterhead and website if you really want to. But if you have aspirations to be a Company Director you might find this aspect of locum work that leads you to question whether you want to be a locum.
Indemnity Considerations
You will probably need to revise your medical indemnity upwards if you engage in locum work. When you work as a locum for a public hospital you should probably still be state government employer indemnified. But it is important to check arrangements each and every time.
Personal Considerations
On a personal level becoming a locum generally means traveling around a lot. Spending time on the road in the car or at the airport. Living out of a suitcase in a hotel or serviced apartment. If you have regular activities like sporting, academic or social pursuits these can be severely disrupted by locum work.
If you have a family you may have some options for them to travel with you to locums. Depending on how needy the hospital or employer is they may even upgrade your accommodation to family accommodation at no extra cost. But at the minimum, you will probably have to pay for them to travel with you. Additional costs such as extra food will probably reduce the financial benefit of doing locums with your family in tow.
Maintaining Registration and Professional Development
I wanted to spend the remainder of this post discussing the issues around continuing professional development for locums.
The Medical Board of Australia has signaled that it will take an increasingly active stance in the process of revalidating doctors (confirming their ongoing suitability to practice) in order to uphold community expectations for quality and safety.
Locum doctors are often left in a vulnerable area when it comes to continuing professional development and demonstrating their ongoing fitness to practice.
And. By the way. As a locum doctor, you are going to also have to think about how you pay for your CPD. Because the hospital is not going to pay for it.
On the other hand, you are probably saving heaps in College fees.
Specialist locums can generally maintain their continuing professional development through their college’s CPD program.
However, locum doctors without fellowship who are simply relying on their general registration face a more difficult set of circumstances as there is generally no professional organization that can fully support their professional development requirements.
Under its Professional Performance Framework the Medical Board has stated that:
All doctors will:
– have a CPD home and participate in its CPD program
Medical Board of Australia
– do CPD that is relevant to their scope of practice
– base their CPD on a personal professional development plan
– do at least 50 hours of CPD per year, that includes a mix of:reviewing performance
measuring outcomes, and educational activities.The current Medical Board requirements for medical practitioners who have general registration only (i.e. do not have specialist registration) indicate that such doctors must
- complete a minimum of 50 hours of CPD per year (self-directed program), which must include
- at least one practice-based reflective element; clinical audit or peer review or performance appraisal, as well as participation in activities to enhance knowledge such as courses, conferences and online learning, or
- meet the CPD requirements of a specialist medical college that is relevant to their scope of practice.
Most doctors can make a plan to engage in courses, conferences and online learning. However, the tradition of clinical audit, peer review and performance appraisal is patchy within medicine in general and it’s likely that locums with general registration may struggle to revalidate if they are unable to plan for these mandated activities each year and possibly have some support for doing them.
Let’s look at each of the mandated practice-based reflections in turn and consider how it might be implemented for a locum doctor.
Clinical Audit
A clinical audit compares actual clinical practice against established standards of practice. The audit has two main components: An evaluation of the care that the individual practitioner provides, and a quality improvement process. The evidence required by the Medical Board is a certificate confirming completion of clinical audit or a short summary of recommendations and implemented changes or a description of the process that was undertaken and a reflection on what was learnt.
Practically engaging in a clinical audit may be difficult for locum doctors because of time constraints for each placement as well as the ability to access and review clinical records at a later point in time.
Peer Review
Peer review meetings are undertaken by and with peers with the aim of updating knowledge and improving practice through the presentation of one’s own work to one’s peers with the expectation of a free and frank review. Evidence of peer review acceptable to the Medical Board includes documented account of case review or discussion with peer or team and a reflection on what was learned or evidence of log book or diary entry and a reflection on what was learned or a description of peer review activity and a reflection on what was learned.
The practical problem for locum doctors engaging in peer review is coordinating meeting times and locations so that peer group members can regularly attend. This might be overcome with the use of technology and holding peer review meetings online. Although it would be important to consider the security implications of online discussions.
An exciting aspect of a locum peer review group would be the potential to incorporate locum doctors working across a range of specialty areas into a group where one could imagine a breadth of generalist knowledge could be imparted throughout the group.
Performance Appraisal
Performance appraisal incorporates activities that allow the practitioner to review their practice /performance. The Medical Board will accept documentation to show how the practitioner reviewed or improved their practice or performance and a reflection on what was learned or a description of the process undertaken and a reflection of what was learned from the appraisal.
In my opinion, this is probably the simplest of the 3 options for mandated peer-based reflection in order to achieve compliance and could be effectively completed with a performance coach.
What the Medical Board Doesn’t Accept as Evidence of CPD
The Medical Board is becoming quite circumspect in relation to CPD evidence. Here is a list of things that the Board will not accept as evidence of 50 hours of CPD per annum.
Receipts of Courses Course Itineraries Course Agendas Course Programs Conference Itineraries Conference Agendas Non planned and non measured reading online Web-surfing Statutory declarations stating 50 hours of journal reading was undertaken Agendas of journal clubs Generally speaking, the Medical Board requires more definitive evidence of the 50 hours of CPD, examples of which would include certificates of attendance, certificates of completion, evidence of questions being attempted and log books of readings.
Related Questions.
What Areas of Medicine Can I Locum In?
Locums can pretty much find work in any area of Medicine these days. At a Consultant level hospitals are often looking for locums in all of the common specialties, including Physicians, Surgeons, Psychiatrists, and Critical Care Physicians. There are also a surprising amount of Medical Administration locums advertised on a regular basis. And of course, there is general practice.
At a non-Consultant level, you can also easily find locums in all range of specialties but critical care (mainly emergency) and psychiatry tend to be the most common along with medical registrar roles.
How Do I Choose a Locum Company?
We have written another post for you on this question. Feel free to have a read of it.
How Long Should I Locum For?
It’s difficult to categorically answer this question. Some doctors have turned locumming into a long term career quite successfully. Some doctors go into locumming planning that it will just be a temporary year or two away from training or permanent work but then find themselves enjoying the work and the lifestyle it provides.
Perhaps the question should be “How Long Should I Locum For. Before I Consider Locumming to Be a Career?” As I have indicated above. Whatever part of Medicine you are in it is important to maintain your standards and professional development.
I’d recommend that if you have been locumming for more than two years then you should review your professional development approach.
Even if you are a Specialist and under a College CPD framework you probably want to think about how working as a Specialist Locum affects you differently than working in a permanent role and a team. Establishing a Peer Review group with other Locums in your Specialty may make sense or perhaps joining an existing Peer Review group of Specialists who work in your field in permanent roles.
As a non-registered doctor, there will come a point where it is difficult to maintain your professional development through a College. There are a few alternatives, such as enrolling in Masters programs at University but the CPD from these programs only lasts as long as the program lasts.
Again a Peer Review group probably makes sense as well as organizing for a regular performance assessment. You should also try to develop a CPD plan at the start of each year to address current gaps in skills and knowledge and consider asking your locum employers for feedback on your strengths and weaknesses.
A career coach may be useful in guiding you through some of these processes.
Is it Possible to Make a Career As a Locum?
Yes. One could make a strong argument for obtaining a Fellowship first to support the locum choice. But there are doctors who have forged a career successfully locumming. At the present time, there is high demand for locums and there has never really been a time when a degree of locum doctors have been necessary to compliment doctors working in permanent roles. As we have highlighted above a key consideration is how you stay current in your practice.
- complete a minimum of 50 hours of CPD per year (self-directed program), which must include
-

Top 5 Medical Job Interview Tips From a Doctor Expert
Would you like 5 tips for preparing for your next medical job interview? Hello, I’m Dr. Anthony Llewellyn, doctor and medical HR expert and I love to share tips with other doctors about how to improve their performance in the job interview.
When approaching a medical job interview or any other job interview for that matter the key things you should consider are:
- Establishing a practice schedule and actually committing to practicing
- Get an understanding of what the panel is looking for, so you can predict the questions you will be asked
- Review your CV for examples of your work that will increase the power of your responses to questions
- Recording yourself practicing so you can see what you actually look like
- Getting feedback on your performance from an expert
These are my top 5 tips based on years of experience in being a recruiter as well as coaching other doctors for job interviews. Let’s dig into them a little deeper.
1. Practicing
This is the most vital tip in my opinion. You should definitely treat the interview as an examination or a performance. I’m betting that throughout medical school you practised and prepared for exams. So why would you expect to just turn up for your next job interview, “wing it” and turn in a great performance?
Your next job is just as important if not more important than getting a pass on an exam. So you need a bit of a practice schedule and you need to actually practice. I recommend giving yourself at least 6 weeks if possible and doing at least one practice session per week prior to your actual interview. If you have less notice of your interview then obviously you will need to condense this and increase the frequency. Better yet. If you are anticipating a new job in the next 6 months. Think about setting up a practice schedule now
2. Understand what the panel is looking for
You need to understand what the interview panel is looking for. So you can practice the right questions and prepare the right examples. I’m often asked by doctors.
“How can I predict what sorts of questions I will be asked?”
Well. Its actually a lot easier than you think.
The questions you get asked in the interview should relate to the Selection Criteria. So to find these go to the appropriate section on the job description and review it. They are usually placed towards the end of the document. These should give you a fair indication of the types of questions you will be asked.
Sometimes, particularly for college selection, rather than selection criteria, there is a competency framework. These are normally easy to find on the college website. Again these will give you a very good guide to what you will be asked about.
You can then generate appropriate questions or there are places online you can find a bunch of them. You can access our free question bank here.
3. Review your CV for examples.
Your CV or resume is a treasure trove of achievements from which to draw upon examples of your past work (or at least it should be). Review your CV for examples so that you can use these as part of your answers to questions.
Remember providing an example from your past work is extremely powerful at the interview.
Dr Anthony Llewellyn, Career DoctorSometimes you will be asked for an example as part of a behavioural question. But don’t be afraid to offer one, even if the question is a hypothetical question.
You are basically telling the panel.
“I can do this. Because I’ve done it before.”
And panels know that past behaviour predicts future behaviour so they will value this information.
4. Record yourself and watch yourself.
Why do I say that you need to record yourself and watch yourself back? Well. Interviews are as much about body language and tone of speech. In fact even more about these things. Than what you say.
So. Its important to know how you appear during an interview.
The only way you will know this is to observe yourself.
Here’s a great example.
Often when I am coaching candidates for an interview I notice that they appear quite stiff in their presentation. This is normally because they are trying to control their hands. By sitting on them or anchoring them in their lap. Actually, you generally want to let your hands get involved in your interview performance. Once we fix this problem. The visual performance always looks a lot better.
There are a number of options for filming yourself for an interview performance. My recommendation would be to use a desktop or laptop set up and record yourself on Skype or Zoom. This way you should easily be able to get at least a head and shoulders view of how you look whilst seated. It’s particularly important to be able to see what you do with your hands.
Alternatively, you can use your smartphone with a tripod if you have one or even just a stack of books on the table. Selfie videos are not as good as you have at least one hand engaged for the filming purpose. Similarly observing yourself in the mirror is not as good as you cannot rewind and go back.
5. Engage an Expert
My final tip is to get some interview practice with an expert.
What do I mean by an expert?
I mean anyone who has had significant experience being a member of a selection panel and/or experiences in coaching candidates for interviews.
Preferably both.
So as a minimum. Try and get someone like a Director of Training or Director of Medical Services to give you a couple of sessions. These people have generally sat in on hundreds of interviews.
Don’t fall into the trap of relying on feedback from fellow candidates, your family or friends. Their feedback is likely to be unhelpful and too much on the positive and encouraging side. Because they have no context for what the panel is looking for and they are too invested in your success and you as a person. You want as critical feedback as possible.
And. If you want to up your game and performance to a higher level.
Then an interview coach is definitely the way to go.
Related Questions.
Question. What if there are no obvious selection criteria?
Answer. There should be selection criteria for any job that is advertised. Sometimes however the job writers or the job writing system make these difficult to decipher. If you have any queries about what the criteria are its best to contact the person whose name is associated with the role for clarification.
Question. How do I find an interview coach?
Answer. There are interview coaches available in most places these days. You can generally do a Google search and someone will pop up. We’ve written an article about how to find a good interview coach that is good for you. Bear in mind that you generally get what you pay for. So the price should not be your only consideration. Also, bear in mind that many coaches can assist you now over the internet. This can sometimes reduce the cost of coaching and give you access to a bigger pool of options.
Question. I get really nervous in interviews. Are there some specific things I can do about this?
Yes. There is. The first thing would be to engage with an expert coach so that you can get some help in improving your overall performance. Practice will help to reduce your nerves on the day. There are specific relaxation techniques that you can incorporate as part of your coaching or separately which will also assist with your performance anxiety on the day.
-

How To Write a Cover Letter Or Email. 5 Sentences May Be All You Need.
If you are applying for a job you may have been asked to provide some sort of cover letter as part of the process. When I say cover letter this might in fact be an email these days or even just some notes as part of the online application process. Many doctors can be confused about the purpose of a cover letter and what to put in. So let’s break it down.
The key issues to address when writing a cover letter or cover email for a job are the following:
- Check if a cover letter or email is even required. Some organizations may specifically request you don’t send in a cover letter or email.
- Make sure that your CV or Resume is tailored to the position and explains how you are a good candidate and meet all the criteria.
- Write a short cover letter or email that specifically mentions the position you are applying for, highlights a key strength you bring to the position and invites the reader to review your CV or Resume.
- Finish your cover letter by indicating that you are open to other suitable positions.
All of the above should take you about 4 or 5 sentences. So the end result will be very brief whether its a cover letter or email. You may have been told elsewhere that the a cover letter should be longer and fully address the selection criteria. But I’m going to show you why the “less is more” approach is better. And also cover some other important issues when writing your cover letter.
Don’t Write a Cover Letter if They Ask You Not To.
This should be a fairly obvious point. But if the hospital or organisation asks you not to write a cover letter. As for e.g. NSW Health does. Then don’t do it.
In the days before the internet and web applications cover letters served a different purpose. One function was for candidates to address selection criteria in writing. However, online recruitment systems now allow you to do this by setting up form boxes to complete.
So if the system says not to submit a cover letter then you should obviously concentrate your efforts on filling in the online application and ensuring that your CV covers the key selection criteria in depth.
Write a Brief Cover Letter. So They Read Your Resume.
Assuming that you have taken the time to properly construct a Resume that is tailored to the position. Then you want the person recruiting to read this document. Your cover letter’s main purpose then is to get them to take that action. And if you put in too much detail they may not take that action.
So try this formula which I partly credit Andy La Cavita for some of the concepts here.
First Sentence
Address your letter or email to the person recruiting.
e.g.
Dear Dr Jones, I am writing to apply for the position of Senior Resident Medical Officer at the Regional Hospital*
*Use the exact title of the position as it reads in the job advert and position
Second Sentence
Tell them why you are a really good candidate for the job. Think about the key strength that you can bring to the role. Is it experience? Is it additional qualifications? Is it something even more unique? For example, for a surgical position, you might something like:
I offer 6 years of clinical experience, including 4 years of excellent performance in surgical registrar roles, which makes me a good candidate for the position.
It is important to finish this sentence by indicating that you are a good candidate. You can use other words like outstanding or great. But the key thing here is that recruiters don’t want to hire mediocre or below average people for their jobs. So signal that you are not one of those candidates.
Third Sentence
If there are any key must haves. Make sure that they know you have these. There are certain requirements for medical posts that you just “won’t pass go” on if you don’t have them. So you want to make sure that these are highlighted to avoid being prematurely culled.
A great example of this is International Medical Graduates applying for positions where an IMG will be considered. Often times employers will want to see that you have met the basic requirements for being registered and therefore eligible to apply. So you might use an example such as:
I have recently completed my AMC Certificate with outstanding marks and I have a current IELTS test score with an average of 8.0. I also hold Permanent Resident status.
For other College training positions a sentence like
I am registered as a trainee with College having made good progress in my training requirements to date.
Fourth Sentence
Let them know about your CV or Resume.
The key here is to create intrigue.
First, obviously, make sure that your Resume is tailored and has a personal statement or career goal statement in alignment with the position.
Then write a sentence similar to the below.
I have taken the time to read the position description and put together a CV that highlights several key strengths that I would bring to this position.
You are telling the recruiter several things in this short sentence.
Firstly, you have taken the time to really consider the job role that they probably wrote and put some effort into. So you are sincere in your interest and not just simply fishing. Secondly, that you have bothered to align your career with that of the job in an effort to demonstrate to the person recruiting how you might be a good candidate. And thirdly, that it will be worth their while reading your CV, because there are some exciting aspects to it.
Fifth and Final Sentence
Close off with a call to action. Your best case scenario is to get a meeting before the proper interview. So aim for this.
I’d welcome the opportunity to speak with you if you feel that I am a good candidate for this job or any other suitable job in the hospital.
You are telling them that you would like a phone call or in person meeting. You are also indicating that you are not just interested in the job but the hospital or organisation in general. Managers and doctors in recruiting roles also like to feel that candidates are seeking out their organisation because of its reputation. Also, there often job opportunities coming up that have not yet been advertised. So you are establishing an insider run for these as well.
And that’s it.
You have now either written a four or five sentence letter or email that:
- Establishes your interest in the job and the organization
- Signals that you are a strong candidate
- Highlights a key strength
- Checks off on any “must haves”
- Intrigues the reviewer to want to read more in your Resume
- Sets you up for an initial conversation
Related Questions.
Question. How Do I Make Sure I Address the Selection Criteria In My Resume?
Answer.
Some criteria will be easy to demonstrate, for e.g. your medical degree and registration status. Just make sure these are listed briefly in the correct section on the front page. You should use the opening personal or career statement on your CV to cover off on the remaining criteria. You may not be able to go into depth for all criteria. Where it makes better sense to do so indicate that certain criteria are covered under your work experience, education etc… and then ensure that you use further narrative in those sections to make your case.
Question. What If They Ask For a Personal Statement or Letter Addressing Selection Criteria?
Answer.
If there is a definite request for a Personal Statement or letter addressing the criteria. Then you should obviously write one. In which case, there is not much sense repeating yourself too much in your CV. Include a briefer personal statement or career statement and then concentrate on other aspects of your CV.
Question. How Do I Find the Selection Criteria?
Answer.
You would think that it would be fairly obvious on a job description what the selection criteria are.
But sadly in my experience, this is not always the case. Sometimes these are listed under the heading Selection Criteria. That heading might read Requirements instead. Sometimes you may also see Sections like Required Skills and Qualifications.
When in doubt you should try to contact the person recruiting to clarify the actual Criteria by which you will be evaluated.
-
Medical Internship 2019 Guide. With 5 Tips For Applying.
It’s that time of the year again. The time when each of the States and Territories in Australia opens up the process of applications for medical internships for the following year. For four years I was responsible for running the largest Intern application system in Australia for 4 years. The NSW Intern application system. So I’d like to share with this year’s medical graduates some of the wisdom I gained from that experience.
(Disclaimer: All information here has been sourced in good faith but things do change so you should always do your own due diligence in such matters, we are providing this information to aid you in your application but take no responsibility for any outcomes)
Intern applications and allocations are coordinated across Australia so that every State and Territory opens and closes their systems at the same time and makes offers at the same times. The key things that all medical graduates should consider in preparing their medical internship application for 2019 are as follows:
- Applications open on 8th May 2019.
- Applications close on 7th June 2019.
- Make sure that you have an Intern Placement Number otherwise you won’t be able to apply.
- You should research the application requirements now as there may be some “surprises”. As soon as the application system opens, register or log in and ensure that you have everything you need to complete your application.
- Understand where you sit in the priority list for any State or Territory you are applying to.
- If you will need to attend an interview. Make sure you have gotten leave from your medical school requirements to attend.
- Give yourself time to request referees, put together a CV and find other documents that you may need.
- First offers come out from 15th July 2019. So make sure that you have regular access to your email as your time for accepting offers can be quite short.
Tip #1. Your Medical Intern Placement Number.
The IPN is a unique nine-digit number that has been generated by AHPRA and has been provided to medical schools for distribution to all 2019 final year medical students. The number is used as part of the national audit process (which ensures that intern positions across the country are made available to as many applicants as possible) as well as to streamline registration.
This number is not the same number as your AHPRA registration number or student number. If you have not received you IPN you should check with your school
Tip #2. Other Things You Will Likely Need.
The majority of States and Territories require you to upload an academic transcript as proof that you are indeed a medical student.
They will also request evidence that you satisfactorily meet the AHPRA English Language requirements. This may seem a bit ridiculous given that you have been attending medical school in English for the last 4 or 5 years. But it is the law. So check whether you may need to submit an up-to-date English test result or some other form of documentary evidence such as a high school certificate.
Most States and Territories will also request a CV or Resume. For tips on your CV or Resume see our ultimate guide to CVs or watch the video below.
Some States and Territories have a CV template that they suggest that you use to fill in your information. In the case of Victoria, you are required to use this template. It’s probably fairly harmless to use the template for the other States and Territories. But if you are thinking about your future career, then nows is a good time to be designing your own CV. The risk of using the template is that you don’t stand out from other candidates.
You will need to also provide proof of your identity, citizenship, residency or visa. And if you have had a name change along the way you will probably also need to provide some documentation in relation to this.
Why All This Information?
The State and Territory bodies who administer the Intern application process have a responsibility to ensure that you are eligible to apply for provisional registration at the end of the year in order to work as an Intern. They collect this information to check that everything is in order so that you are indeed eligible to apply. Employers can get rightly annoyed when told that someone who has been allocated to work with them as an Intern will have a several-month delay whilst they resit an English language test.
However, it’s your responsibility to ensure that you are eligible for registration. So you should also be checking these things yourself.
Tip #3. Research and Apply Early.
It’s hard to fathom given the amount of communication from health departments, medical schools, and student colleagues. But every year there are a handful of medical students who forget to apply for their internship. This means having to wait another year. Don’t let that be you.
There are even more students who leave their applications to the last minute. Only to find that they are missing a vital document. For example, this could be evidence you need to substantiate that English is your first language, such as a high school certificate. Or perhaps your last name has changed whilst you have been in medical school? Or maybe you need to submit a CV with your application?
As soon as the application page opens for each State and Territory you are going to apply to make sure your register. And then go as far through the process of applying as possible so you can see if there is some sort of document you need to obtain.
Tip #4. Know Where You Sit In The Priority List.
It’s important to know where you sit in the priority list. Each State and Territory has a slightly different order but in essence, it goes something like this:
- If you are an Australian Citizen or Permanent Resident and went to Medical School in that State or Territory you are top of the list.
- If you are an Australian Citizen or Permanent Resident and went to Medical School in another State or Territory or New Zealand you are probably second.
- If you are an International student who studied Medicine in Australia you are probably next.
Priorities Within Priorities.
Some States and Territories also have priority pathways to ensure that groups such as Aboriginal and Torres Strait Islanders and doctors who wish to work rurally or regionally can obtain their preferred placement early.
So if you are an International student and like the idea of working rurally its probably a good idea to consider a rural pathway as it will likely boost your chances of gaining an Intern position earlier in the process.
South Australia
Intern Positions ≅ 260
Annual Salary = $73,370
Intern Positions in South Australia are administered via SA Health Careers
Northern Territory
Intern Positions ≅ 50
Annual Salary = $71,350
In the Northern Territory Internship is organised by the Northern Territory Prevocational Medical Education Assurances Service.New South Wales
Intern Positions ≅ 1,000+
Annual Salary = $67,950
Intern Positions in New South Wales are administered via HETI.
Victoria
Intern Positions ≅ 820
Annual Salary = $74,639
Intern Positions in Victoria are managed by the Postgraduate Medical Council of Victoria
Commonwealth Program
Intern Positions up to 115
Annual Salary = uncelar
The Commonwealth provides an additional Internship program for international students who study at Australian medical schools.
*Any excess posts may be applied for by other IMGs in Australia
Western Australia
Intern Positions ≅ 310
Annual Salary = $78,749
In Western Australia Intern Applications are coordinated by the Postgraduate Medical Council of Western Australia (PMCWA).
Queensland
Intern Positions ≅ 840
Annual Salary = $73,306
Intern Positions in Queensland are administered via Queensland Health.
Canberra
Intern Positions ≅ 95
Annual Salary = $68,094
Intern Positions in ACT are administered by ACT Health.
Tasmania
Intern Positions ≅ 90
Annual Salary = $68,936
Intern Positions in Tasmania are administered by the Department of Health and Human Services.
Western Australia.
Annual Salary = $78,749
Estimated Numbers = 310
In WA all interns are employed by a Primary Employing Health Service (PEHS).
There are 4 PEHSs and each PEHS is a major tertiary hospital in WA which have been accredited to directly employ interns and provide a high-quality intern training program.
Each PEHS holds an information night.
You can also choose to work as a rural intern by applying to work through Western Australia Country Health Service.
The process is coordinated by the Postgraduate Medical Council of Western Australia but you apply through the WA Jobs site and selection occurs through panels representing each of the PEHSs.
As part of your application, you need to provide a cover letter and CV and will require a range of other documents as well as to nominate 3 referees.
If successful you will receive a contract for 3 years.
Northern Territory.
Annual Salary = $71,350
Estimated Number = 50
The NT Prevocational Medical Assurance Services (PMAS) conducts a central review of eligible applicants and all intern positions are allocated within the two NT Health Services:
- Top End Health Service (TEHS) – Royal Darwin Hospital (RDH)
- Central Australia Health Service (CAHS) – Alice Springs Hospital (ASH)
Eligible applicants are allocated intern positions in line with the Northern Territory category groups. Within the relevant category groups, applicants are allocated to their highest possible Health Service preference, pending availability of a position.
Overall the intern allocation process is based on an applicant’s category group, Health Service preference, and the number of positions available in each health service.
The two NT Health Services are responsible for selecting applicants and making their offers of employment, applicants are advised via email. The Health Service responsible for making the offer of employment will after receiving an acceptance from an applicant arrange an employment contract for an Internship position within their health service to be provided prior to commencing the internship.
NT Department of Health Intern Recruitment Link (includes information on Categories)
South Australia.
Annual Salary = $73,370
Estimated Number = 260
SA Health Careers conducts the annual Intern application process in South Australia.
There are 3 Adelaide-based Local Health Networks and one small Country Health Network (based at Mt Gambier & Whyalla) to which you can apply for the priority Rural Intern pathway.
The Rural Intern Pathway is a strength-based recruitment process for applicants who are interested in undertaking their internship (and potentially subsequent years) in rural hospitals within Country Health SA (CHSA). Rural intern positions provide broad opportunities in unique settings and are best suited for medical graduates with a history of living or working in rural areas or a desire to commence a career in the country.
Intern Allocation Priorities:
- Category 1 Australian Citizens, Australian Permanent Residents and New Zealand Citizens
1.1: Medical graduates from a South Australian university who identify as Aboriginal and Torres Strait Islander (ATSI)
1.2: Medical graduates from a South Australian university – Commonwealth-supported (HECS-HELP) or SA Bonded Medical Scholarship Scheme (SABMSS)
1.3: Medical graduates from a South Australian university – full-fee paying- Category 2 Australian Citizens, Australian Permanent Residents and New Zealand Citizens
2.1: Medical graduates from an interstate or New Zealand university who identify as Aboriginal or Torres Strait Islander (ATSI)
2.2: Medical graduates from interstate or New Zealand university who completed Year 12 in South Australia
2.3: Medical graduates from an interstate or New Zealand university
2.4: Medical graduates from an overseas university who completed Year 12 in South Australia
2.5: Medical graduates from an overseas university- Category 3 Australian Temporary Residents and New Zealand Permanent Residents
3.1: Medical Students from a South Australian University
- Category 4 Australian Temporary Residents and New Zealand Permanent Residents
4.1: Medical graduates from an interstate or New Zealand University
- Category 5 Australian Temporary Residents and New Zealand Permanent Residents
5.1: Medical graduates who have spent two or more semesters in an overseas campus of an Australian or New Zealand University (eg Monash Sunway campus, UQ New Orleans campus)
5.2: Medical graduates of an overseas universitySouth Australia is one of few States that specifically permits medical graduates from other countries to apply for internship positions. But they are at the very bottom of the priority list.
If you are not a South Australian medical student, in order to apply for an internship in South Australia you will need to provide a certificate confirming that you have completed the SA Health online electronic medical record (Sunrise EMR & PAS) training.
SA Intern Application Job Pack (with priority categories
Queensland.
Annual Salary = $73,306
Estimated Numbers = 840
Queensland Health conducts the annual intern allocation process in Queensland.
Interns can be allocated to one of 19 hospitals.
An interesting aspect of the Queensland application portal is that you can see a live indication of where other applicants have preferenced other hospitals. This is presumably designed to encourage medical students to consider other hospitals and get the student group itself to work out the allocation.
I have no indication whether it’s a useful process or not. If you know anything about this. Leave a comment below.
Intern Allocation Priorities:
Group A
Medical graduates of Queensland universities who are Australia/New Zealand citizens or Australian permanent residents; and- are seeking an internship commencing in the year immediately following graduation; OR
- received Review Committee approval from a previous campaign to defer commencement of internship
Group B
Medical graduates of Australian (interstate) or New Zealand universities who are Australian/New Zealand citizens or Australian permanent residents;
OR
Medical graduates of Queensland universities who are Australian/New Zealand citizens or Australian permanent residents who do not meet the criteria outlined in Group AGroup C
Medical graduates of Australian (Queensland or interstate) or New Zealand universities who are NOT Australian / New Zealand citizens or Australian permanent residents who:- currently hold a visa that allows them to work in Australia; OR
- will need to obtain a visa to work in Australia
Group D
Medical graduates of Australian University campuses outside of Australia accredited by the Australian Medical Council.
OR
Medical graduates of international universities who have not completed an internship in Australia or another country and have either:- obtained the AMC Certificate (and are eligible for provisional registration)
- successfully completed the AMC MCQ (multiple choice questionnaire) (and are eligible for limited registration)
The Queensland Rural Generalist Pathway (QRGP) offers graduating medical students the opportunity to explore a wide variety of clinical training and develop the advanced skill set required to support the health needs of rural communities. It’s a priority pathway that you can opt for first.
If you are not interested in the Rural Generalist pathway then you need to work out which category you are in.
New South Wales.
Annual Salary = $67,950
Estimated Numbers = 1000
The Health Education & Training Institute runs the countries largest Intern application process. Offering over 1,000 internships.
Interns can be allocated to one of 15 networks of hospitals. The offer is for a 2-year contract to cover both internship and residency.
You have the option of applying through one of 4 pathways:
- Aboriginal Recruitment Pathway
- Rural Preferential Pathway
- Regional Allocation Pathway
- Optimised (or Main) Pathway
Only applicants who go through the Rural Preferential Pathway need to submit a CV and attend an interview. All other pathways are based on applications only.
Intern Placement Priorities:
Priority 1 – Medical graduates of NSW universities who are Australian/New Zealand citizens or Australian permanent residents (Commonwealth Supported Place and Domestic Full Fee paying).
This priority category is guaranteed an intern position in NSW.
Priority 2 – Medical graduates of interstate or New Zealand universities who completed Year 12 studies in NSW who are Australian/New Zealand citizens or Australian permanent residents (Commonwealth Supported Place, Domestic Full Fee paying or NZ equivalent).
Priority 3 – Medical graduates of interstate or New Zealand universities who completed Year 12 studies outside of NSW who are Australian/New Zealand citizens or Australian permanent residents (Commonwealth Supported Place, Domestic Full Fee paying or NZ equivalent).
Priority 4 – Medical graduates of NSW universities who are not Australian/New Zealand citizens or Australian permanent residents and who hold a visa that allows them to work or are able to obtain a visa to work.
Priority 5 – Medical graduates of interstate or New Zealand universities who are not Australian/New Zealand citizens or Australian permanent residents and who hold a visa that allows them to work or are able to obtain a visa to work in Australia.
Priority 6 – Medical graduates of Australian Medical Council accredited universities with campuses that are located outside of Australia or New Zealand who are not Australian/New Zealand citizens or Australian permanent residents and who hold a visa that allows them to work or are able to obtain a visa to work in Australia.
HETI Medical Graduate Recruitment Page.
HETI Prevocational Training Application Program Portal.
Australian Capital Territory.
Annual Salary = $68,094
Estimated Numbers = 95
(6 of these positions are normally guaranteed to NSW medical students)
If you want to apply for an internship position in the Australian Capital Territory you do so via the ACT Health Recruitment page.
Most of your time is spent at the Canberra Hospital. But ACT is interesting as it is one of the few chances you may have as an Intern to work in 2 separate States and Territories. Rotations may include secondments to Calvary Public Hospital, Goulburn Base Hospital, and South East Regional Hospital (SERH) at Bega.
Other details are limited at this stage.
Victoria.
Annual Salary = $74,639
Estimated numbers = 820
Internship in Victoria works around a computer matching system which is administered by the Postgraduate Medical Council of Victoria.
Once you have submitted all your details and preferences the match informs the various hospitals and health networks who then conduct a selection process. Some but not all hospitals and networks perform interviews. Your selection may just be based on where you sit on the priority list plus your CV and referee reports.
Interns can be allocated to one of 22 hospitals and networks. This includes a small number of community-based internships where the focus is more on community-based models of care, including working in primary care and smaller hospitals.
For Victoria, you will need to submit a CV. This MUST BE on the quite unattractive PMCV Standardised CV Template. You don’t have to put a photo on your CV. And I would not recommend doing so.
Intern Placement Priorities:
Priority Group 1 – Australian permanent residents or citizens and New Zealand citizens graduating from Victorian medical schools including CSP and domestic full fee-paying students (i.e. graduates of University of Melbourne, Monash University, Deakin University and University of Notre Dame: Melbourne & Ballarat Clinical Schools).
Priority Group 2 – Australian temporary resident graduates of Victorian medical schools Interstate Special Consideration candidates (approved by DHHS)
Priority Group 3 – Australian permanent resident graduates of interstate or New Zealand universities (including previous residents of Victoria); Australian temporary resident graduates of interstate universities; New Zealand temporary resident graduates of New Zealand universities; and Graduates from an overseas campus of an Australian/New Zealand University accredited by the Australian Medical Council (e.g. Monash University – Sunway Campus, Malaysia)
Tasmania.
Annual Salary = $68,936
Estimated Number = 90.
Internships are coordinated in Tasmania via the Department of Health and Human Services.
All applicants are required to apply online. As part of your application you are asked to preference all of the 3 available sites:
- Hobart
- Launceston
- North West Region
Candidates need to attach a CV/Resume and any other relevant information to their application and must arrange completion of two electronic referee reports:
One (1) referee that is employed in a clinical role (Clinical Academic) with the University where you are studying/or studied medicine and is aware of your studies in the past 12-24 months; AND
One (1) that is – a senior clinician (>4 years’ experience post general registration) who has observed you (you have worked with) during your clinical placements in the past 12-24 months, and can comment on your suitability for hospital-based practice.
Intern Placement Priorities:
The Tasmanian Health Service currently gives priority, in order, to:
- Australian permanent resident Tasmanian-trained Australian Government supported and full-fee paying medical graduates.
- Australian temporary resident Tasmanian-trained full-fee paying medical graduates.
- Australian permanent resident interstate-trained Australian Government supported and full-fee paying medical graduates.
- Australian temporary resident interstate-trained full-fee paying medical graduates.
- Medical graduates of an Australian Medical Council accredited overseas University.
Selection occurs via face-to-face interviews. Following the interview, successful applicants will be placed in an order of merit with applicant performance at the interview accounting for 70% of the overall score, and each referee report accounting for 15% of the overall score. Vacant positions are offered in order of merit and the Tasmanian Health Service Priority Placement Framework.
Tip #5. Commonwealth Program.
Annual Salary = uncertain.
Likely to be based on the Award for the State that you are working in.Number = up to 115.
The Commonwealth Internship Program is my final tip.
This is because it is a program that runs separately and in addition to the State and Territory internship programs. And you may have not been informed of its existence OR thought to apply for it.
The main function of this program over the years has been to provide additional opportunities for international students studying Medicine in Australia a chance to complete their internship. This is done by tendering to various private hospitals for additional intern positions.
The program has been retitled this year as the Junior Doctor Training Program Private Hospital Stream and there will be a total of up to 115 positions on offer.
Normally there is not as much information about the program available until a mad flurry at the end of the year. And 2019 seems to be no different. They are still sorting out which hospitals will provide internships. After which there will probably be some information about how to apply.
For now, we know that the eligibility requirements are that you must either be an international full fee-paying medical graduate from an onshore Australian medical school. This is Priority One. If not all positions are filled by priority one medical graduates then the private hospitals may then recruit other medical graduates who are eligible for provisional registration. This is the Priority Two category.
Eligibility Requirements for Intern (PGY 1) Junior Doctor Training Places under the Junior Doctor Training Program Private Hospital Stream
Under the PHS, participating private hospitals must prioritize international full fee-paying medical graduates from onshore Australian medical schools (Priority One). Should these places not be filled, private hospitals may then recruit other medical graduates eligible for provisional registration (Priority Two).This means that the Commonwealth Scheme provides one of the few opportunities for IMGs who are applying via the standard pathway process to gain an internship position in Australia.
To do so you will need to have met the Medical Board of Australia provisional registration requirements as a medical practitioner. And also have met the English language proficiency requirements for registration purposes. And commit to obtaining an appropriate visa to work in Australia during the internship year.
Private Hospitals participating in delivering the Private Hospital Stream in 2019 are:
- Mater Health Services North Queensland Limited
- Mercy Health and Aged Care Central QLD
- MQ Health (Macquarie University Hospital)
- St John of God Health Care Inc.
- St Vincent’s Private Hospital Limited
- St Vincent’s Private Hospital Sydney
- Ramsay Health Care
- Greenslopes Private Hospital
- Joondalup Hospital
How To Decide?
There are lots of considerations when it comes to putting in your Intern application. Everyone is a bit different. Some graduates feel like they would like to be close to home and family whilst going through their transition to Intern. Others see it as a chance to get away and explore a new place and location. And then others focus on the long-term career prospects of certain locations.
I think this last consideration is a little overrated for most. You can generally experience a wide range of medicine in your first couple of years of medicine after graduation and there is scant evidence that this affects your prospects of applying for specialty training posts.
That being said if you have an interest in anything other than Medicine, Surgery or Emergency Medicine as a future career you should probably investigate whether this particular specialty is offered at the hospitals or networks to which you apply.
Unfortunately, the internship model in Australia is quite antiquated and we have used the experience as a proxy for competency. The result has been the mandating of the 3 core terms for internship of Medicine, Surgery, and Emergency Medicine. There is really no solid educational basis for this approach and one of the unfortunate outcomes is that all the other specialties get squeezed out and few interns get to experience psychiatry, general practice, obstetrics, paediatrics, pathology etc… which ultimately does have an effect on recruitment to these specialties.
So the basic message is this. If you are really dead set keen on doing radiology as a career you should try to track down the very few locations that might offer this rotation to either interns or residents.
Each year the Australian Medical Students’ Association produces a very useful Intern Guide with lots of information about the composition of intern training networks across the country. We are currently waiting on the 2019 version. But here’s a link to the 2018 version.
Related Questions
Question: What If I Have Special Circumstances Which Make It Hard For Me To Work In Certain Places?
Answer: All States and Territories Have processes for considering special circumstances. Some of the types of circumstances that are generally approved are: where you may have certain health conditions that mean you need to be close to certain hospitals or specialists; where you have dependents, such as young children, and are unable to relocate due to care arrangements; and where you and your partner want to work as doctors in the same location.
Generally, requests to stay in certain locations, for reasons such as work commitments of partners or needs of school aged children are not granted.Question: I Have Received My Intern Offer. But I Would Like to Defer It. Is This Possible?
Answer: This will partly depend on how long you wish to defer for.
If you just wish to defer for a a few months. Once you have your offer and are in discussions with your new employer make enquiries. It may be possible to negotiate a later start with your employer. Most employers will generally prefer that you start on time, so that you are not out of sync with your colleagues. But there might be some advantage for the employer in you attending orientation but then starting a bit later as it will probably help them to fill out roster gaps.
On the other hand. If you wish to defer for a complete year. Then you will need to check the policy of the State or Territory that has provided you an Intern offer. In some cases (for example Victoria) you will be permitted to defer and your place will be held for you the following year. In most other cases you will need to reapply the following year and check whether your priority status has altered. In most cases you have the same priority status.
Also bear in mind that it is unclear how long you can defer commencing your internship. However, the Medical Board of Australia expects that once you have commenced your internship you will have completed this process within 3 years.Question: I Am a Doctor With a Medical Degree From Outside Of Australia. Can I Apply For Internship?
Answer: Unless you obtained your medical degree from a New Zealand Medical School. Then the brief answer to this question is no.
I would love to stop there. And I really think you should as well. But there are rare circumstances where you may be able to obtain an internship with a medical degree from outside of Australia. But the Medical Board of Australia strongly advises against this option and so do I. For good reasons. Firstly the whole Australian medical internship system is designed to ensure that Australian medical graduates are able to undertake an internship. Not for overseas graduates. Secondly (and as a result of the first point) it is very rare to be offered the chance.
Some States and Territories will not even consider an application from an IMG for internship. Others will only do so in limited circumstances, for example, the Northern Territory will accept applications from IMGs who may have done a medical student elective or clinical observership in the Northern Territory and who have experience in rural, remote and indigenous health locations. But even then these applicants are at the bottom of the priority list for obtaining an internship. South Australia will accept applications. But again you are bottom of the list. Queensland will also accept applicants, but only if you have never worked as a doctor. And again you are bottom of the list.
A final note on this question is that the majority of IMGs who do obtain a medical internship position each year in Australia generally have Australian citizenship or permanent residency.Question: I Have Heard That Some Graduates Miss Out On Internship. Is This True?
Answer: Whilst it is theoretically a possibility that some medical graduates miss out on Internship according to information provided by HETI for the most recent year of intern applications no-one was actually left at the end of the process without an offer.
Only Australian citizens and permanent residents are guaranteed an intern position under the COAG agreement. However, there are generally enough intern positions available for those students who have come to Australia to study medicine and the Commonwealth Private Hospital program offers additional spaces for those that may miss out.
That being said. It is also clear that many graduates choose to drop out of the application process themselves. So not everyone who applies gets an offer. The assumption is that some graduates take up similar intern opportunities in other countries upon graduation.
(Disclaimer: all information here has been sourced in good faith but things do change so you should always do your own due diligence in such matters, we are providing this information to aid you in your application but take no responsibility for any outcomes)
We’d welcome feedback from any Intern programs in relation to the accuracy of the above information. -

How Much Do Specialty Trainee Doctors Earn? Registrar Pay Rates
On this blog, we want to give you the best information possible about Medical Careers. That obviously includes information about pay rates and related conditions We have already given you the low down on Interns and Residents, as well as Specialists. So its high time we discussed Specialty Trainees or registrar pay rates. Right?
In this post we are going to talk about Specialty Trainees, also referred to as Registrars and how much they earn. Specialty Trainee Registrars working full-time in the hospital system will earn between $89,649 as a first-year Registrar in Tasmania up to $161,766 per annum working at the most senior Registrar level in Western Australia. General Practice Trainee Registrars working full-time are guaranteed $75,328 per annum in their first year of training. Going up to a guaranteed $96,724 per annum in their 3rd and final year of training.
Once again it’s important to emphasize that these salaries are base salaries for full-time employees. Specialty Registrars are often required to work considerable amounts of overtime and on-call which will increase their pay rate significantly. And General Practice Registrars are able to negotiate with their employers above the guaranteed rate of pay. Often this will be on the basis of a proportion of the Medicare revenue that they generate for the practice. So, again they can possibly earn significantly more.

Specialty Trainees Can and Often Do Earn Much, Much More.
We can see evidence of the fact that Registrars do earn much more than their base rate of pay. “Other Medical Practitioners”, which is where most Registrars classify themselves for tax purposes with the Australian Tax Office earned on average $204,387 of taxable income in 2016/17 according to the ATO.
Whilst these figures are likely to be conflated by General Practitioners and other Specialists indicating this category as their profession as well they do back up the contention that most trainee doctors earn significantly more than their base registrar pay rates due to working excessive hours with specialty trainees at most risk of working excessive hours and amongst these Intensive Care and Surgical trainees being at the highest risk of fatigue.
Its certainly been my observation over the years that surgical trainees in particular work long hours. This is generally a combination of rostered and unrostered overtime as well as being “on-call”. I was literally at a meeting last week where an administrator reported that the surgical trainees at her hospital were the best paid doctors last year due to their workload. Meaning that they were paid even more than the specialists.
Its easy to see why and how this would be the case. Lets take a typical situation of a medium hospital which employs 3 General Surgical trainees. Each is on the roster approximately 1 in 3 on top of their normal 40 hours per week. This means being on call around 2 weeknights per week and 1 weekend in 3.
Let’s assume one of these surgical trainees does slightly more than their share of weeknights in a month (4 weeks). 8 in total. But only one weekend. Let’s say that they get called on average 2 times per weeknight and 15 times over the course of that weekend.
In New South Wales each of these call-backs would amount to a period of 4 hours of overtime. This is initially paid at time and a half for the first two hours and thereafter double time.
So we have:
- 160 hours of normal time
- 2 callbacks X 8 = 64 hours of overtime for the weeknights
- 15 callbacks for the weekend = 60 hours
This gives us a total of 284 hours for that 4 week period. Which is close to double the base hours! But wait. Because those overtime hours get paid initially as time and a half and then very quickly as double time. The total amount of hours paid becomes about 400 hours!
So you see it’s not all just about the base registrar pay rate.
Now, this example is obviously not typical for every specialty and there are some specialties that may not have to do as much overtime and not get called in as much. But it is also not the most extreme example either as the case of Dr. Yumiko Kadota has demonstrated to us.
Breakdown of Registrar Pay Rates and Other Rates By State and Territory.
We have compiled below a table that demonstrates the current base rates of pay for Intern, Resident, Senior Resident, Registrar and Senior Registrar for each State and Territory in Australia.
Please bear in mind a number of things. Once again we are talking Full-Time Annual Salary. Also, as I have pointed out above the actual take-home pay can vary considerably. Also, the Awards and agreements for each State and Territory are set independently and at different times from each other. So over time, the tendency is for there to be movement both up and down through the table.
What is apparent, however, as we have pointed out on our other blog posts about Interns and Residents is that Western Australia is clearly the best place to work if your sole interest is registrar pay rates. Victoria is next best and rates a special mention as its Enterprise Agreement contains a lot of additional friendly provisions that others do not.
$31,000 in difference between the highest rate of pay between Western Australia and Tasmania is a bit hard to fathom and justify. It’s almost a 20% difference.
State / Territory Intern Resident Senior Resident* Registrar Senior Registrar** Western Australia $78,479 $86,328 $94,960 $109,678 $161,766 Victoria $74,563 $79,391 $86,060 $116,460 $155,477 New South Wales $67,950 $79,648 $87,603 $99,218 $139,900 Australian Capital Territory*** $68,094 $79,682 $87,410 $98,704 $138,667 Queensland $73,306 $79,413 $85,521 $105,377 $134,389 Northern Territory $71,350 $82,731 $88,629 $98,413 $134,113 South Australia $73,370 $80,041 $86,710 $100,717 $133,400 Tasmania $68,936 $72,837 $89,649 $89,649 $126,854 *Being appointed to a specialty trainee position does not automatically mean appointment to a Registrar role in all States and Territories. For some, for example NSW, the entry point is the Senior Resident Medical Officer position.
**Not all States and Territories have a Senior Registrar role. We have used the maximum Registrar pay grade where there is no Senior Registrar role.
***The Australian Capital Territory Enterprise Agreement expired in July 2017. Therefore we expect that the salaries quoted here will increase significantly when there is a finalization of the new agreement.
What About General Practice?
Ok. So far I have ignored General Practice. But this has not been deliberate. It’s because General Practice is a different set of circumstances to the other specialty training cases. This is because General Practice works more on a national basis. Because there is an Australia-wide minimum set of pay standards.
So, according to the General Practice Registrar Association website the current base rate of pay for a first-year General Practice Registrar is $75,328.23 per year and for a Registrar in their final year (which is either 3rd or 4th year) $96,724.43 per year. Again, this is for full-time work.
Now, whilst these rates appear to be somewhat lower than for Specialty Trainees paid as Registrars you should bear in mind four things about General Practice training.
The first is that General Practice training is a minimum of 4 years, whereas most other specialties are 5 years and possibly longer. So there is no need for higher Registrar levels in general practice.
The second is that is actually possible to enter General Practice training in your PGY2 hospital year. So when you enter your first actual GP training post you are actually in your second year of training.
The third is that the pay agreements are a minimum standard as part of an employment contract below which your employer may not go. But it is quite common for GP trainees to negotiate a better agreement with their employer, by agreeing to collect a share of their Medicare billings. So it is possible to do far better than these minimum amounts. Although, clearly this partly has to do with your own productivity as a GP trainee. And I don’t have any meaningful information to tell you how much this can increase salaries.
The fourth and final thing is that clearly, GP trainees become specialists earlier. So whilst other specialists can and do eventually earn more than GPs. You get there first as a GP and so you get a head start on the rest of the field. Also, GPs are generally working less time than other specialists. So in theory more able to enjoy their very reasonable salary.
Time To Complete Training and Other Costs.
It has been suggested to me by my readers and viewers that in order to tell the complete picture I should talk about the time it takes one to complete training as well as some of the other costs involved in getting there.
Whilst I agree that this probably does make the picture a little bit more complex for Specialty groups such as Surgeons. As I have also pointed out. Whilst one is working as a Surgical Trainee, either accredited or unaccredited you are in a group of doctors who are going to be earning quite a bit due to the amount of time worked. Now. This observation in itself is not really an attractive reason to enter Surgical training in my opinion.
But it does mean that if you are successful in getting your way through Surgical training to your FRACS you are probably going to end up earning one of the highest incomes of doctors across your medical career.
This is all pretty relative when we consider that most medical professions are in or close to the top ten occupations in terms of average income in Australia.
Some key things to observe here are:
- Some specialties are somewhat easier to get into at an earlier stage of training, examples being Emergency Medicine, Psychiatry, Physician Training and Emergency Medicine.
- Other specialties have long waiting lists where you might end up becoming a very, very senior Resident before you get onto the program. Examples here are Surgery, Ophthalmology and Dermatology
- Costs of training fees and exam fees can also vary significantly. Annual College fees usually start at over a thousand dollars for most Colleges. Examination fees can be a few thousand dollars to over ten thousand dollars. These costs are all tax deductible.
- You may also need to or find it desirable to enter a formal training course. Some Colleges make this mandatory. This will also cost you a few thousand dollars. Again. This is also tax deductible.
- Depending on your specialty there may be some equipment that you need to buy. For example, some of the surgical specialties utilise special equipment (think Ear, Nose and Throat).
Other Related Questions.
Question: What Other Benefits Do You Get As a Specialty Trainee?
Answer.
There are a range of other benefits that you get when working as an employed doctor in Australia.
- On top of your salary, your employer is required to pay an additional 9.5% into a superannuation fund to assist with your retirement.
- As an employee, you are covered by workers compensation for any injury or accident that might occur at work. Although payouts are often fairly poor and below what most professionals earn. So you may wish to consider taking out additional income protection insurance.
- If you are asked to be on-call you will get a small allowance for this and be paid if you are called back into work.
- You may get an allowance or even a mobile phone provided to you if you are required to be on call.
- You might get some meal allowances for shifts.
- If you have been seconded a reasonable distance from your normal place of appointment you will generally be provided with free temporary accommodation (you may need to pay a bond) and a travel allowance, for example, a free air ticket back home every 13 weeks or so.
- You will get at least 4 weeks of annual leave per year.
- Most doctors will also get one extra day off per month. Called a Rostered Day Off or RDO.
- You will get a certain amount of sick leave every year which you can accumulate if you don’t use.
- You also get access to other types of leave, such as leave to take your child to the doctor.
Question: If I Am a Specialty Trainee From Overseas. How Much Will I Get Paid?
Answer.
You should be paid the same as the equivalent doctor in Australia. But this is a case where it’s always best to check. Once you are offered a position you should make sure that the employer is taking into account your current status as a trainee doctor overseas and in particular the amount of years of experience you have had. Some employers may indicate that they only take into account years of clinical experience worked in Australia. This can be a grey point. When pushed they will generally recognise your overseas experience as well.
Special thanks to Dr Rachel Seaniger for the research conducted on this post
-

Salary of Australian Doctors | Doctors Pay Scale
Not surprisingly, one of the more popular topics on this blog is the subject of income or salary of Australian doctors. We have recently written about how much an Intern is paid and how much a Resident is paid. Of particular interest to many is how much a doctor earns when they have completed all their training and achieves the status of a Surgeon or a Physician or a General Practitioner or one of the many other specialties in Australia. A recent report from the Australian Tax Office has confirmed that doctors in Australia are amongst the best paid in the country.
If we take our entry point as internship and our peak point an Australian surgeon. Then a good guide as to how much one can earn as a doctor in Australia is somewhere between $68,000 AUD and $395,000 AUD per annum.
Of course not every doctor will earn $395,000 per annum and there are many factors that affect the earnings of a doctor. And a number of doctors also earn even more than $395,000. Let’s dive into the earnings in a bit more detail and also look at some of the cost factors for doctors.
Surgeons, Anaesthetists, Physicians, Psychiatrists and ‘Other Medical Practitioners’ Amongst the Top Ten Earners in Australia.
What is impressive is that 5 of the ten top occupations by earnings come from the medical profession, with Surgeons leading with an average taxable income of $394,866, followed by Anaesthetists in second with $367,343 and Internal Medicine Specialists in third with $299,378. Psychiatrists are in fifth with $216,075 and ‘Other Medical Practitioners’ in sixth with $204,387.
Occupation Average Taxable Income Surgeons $398,866 Anaesthetists $367,343 Internal Medicine Specialists $299,378 Financial Dealer $261,008 Psychiatrist $216,075 Other Medical Practitioner $204,387 Judicial / Legal Professionals $195,703 Mining Engineer $167,345 CEO or Managing Director $157,643 Engineering Manager $147,451 This is even more impressive when one considers that the ATO lists around 1,100 occupations to select from when one compiles their tax return.
You have probably already spotted one potential problem with these figures, which is that they rely on the person completing the tax return to select the appropriate occupation.
The other possible occupations for doctors to choose under the ATO categories are: General Medical Practitioner and Doctor specialist – type not identified. Both of which earned about $140,000 AUD per annum in 2016/17.
Presumably most surgeons select surgeon for an occupation and anaesthetists select anaesthetics etcetera. However, its not clear what occupations trainee doctors select. Most will likely select “Other Medical Practitioner”. Some may select the specialty that they are training in and this will reduce the overall average as trainee doctors earn less than specialists.
There were 28,307 doctors who selected “Other Medical Practitioners” in 2016/17, versus for e.g. 3,951 for Surgeons, so this number would incorporate most of the trainee doctors in Australia. But it might also be joined by for e.g. Emergency Physicians and Obstetricians and Gynaecologists, who don’t have another obvious occupation to select. Not many doctors selected Doctor specialist -type not identified (only 37).
In any regard its fairly plausible to say that trainee doctors are also in the top ten earners in Australia. And this certainly stacks up when one considers the publicly available information about trainee doctor salaries in Australia and one factors in overtime.
The average of these salaries will also be influenced by doctors working part-time and doctors working in the public sector (although as we show below by not too much).
Some interesting information is discerned when one digs into the detail provided by the ATO.
The ATO provides more detailed breakdowns on a State or Territory level so let’s look at Surgeons, Anaesthetists, Physicians and Psychiatrists in NSW:
Occupation Average taxable income Average salary or wage income Average total income Surgeons $324,965 $65,881 $340,511 Anaesthetists $335,301 $68,794 $348,323 Physicians $283,577 $63,489 $296,034 Psychiatrists $213,160 $58,305 $224,159 So what we notice here is that there is a very low level of average salary or wage income compared to the actual salary. This likely reflects the fact that many specialists do not earn the majority of their income as a paid wage but rather through contractual work and Medicare and private billings.
Is There a Difference Between Public and Private Earnings in the Salary of Australian Doctors?
In short. Yes. But what we see when we compare the above average taxable income with some of the rates that Specialists are paid in Australia for working in the public hospital system is something quite comparable.
Let’s take NSW again.
Salaried Staff Specialists.
First, let us look at Staff Specialists. These are Consultants who are employed on a salary basis in NSW hospitals. Generally, they work full time in the hospital system and don’t work in the private sector.
They may, however, see some private patients within the hospital system for which there is sometimes the capacity to share in part of the revenue.
A first-year Staff Specialist working full time will earn a minimum of $234,556 if they do not see private patients. So we are already above the average taxable income of a Psychiatrist.
This income can go up to $342,060 if the doctors sees a large number of private patients and splits this revenue with the hospital. Going past the average taxable income of Physicians.
The staff specialist rates increment every year until year 5. Once you have worked as a Staff Specialist for 7 years you are eligible to apply for Senior Staff Specialist status.
At this point, you will earn a minimum salary of $316,891 and a maximum salary of $462,133.
At this point, the Specialist is on par with the average taxable income of a Surgeon.
Add to this a generous professional development allowance of up to $35,000 and the possibility of a managerial allowance of an extra $9,000 to $23,000 for being the head of department or such. Being publicly employed is a well-remunerated experience for specialist doctors.
Visiting Medical Officers.
Visiting Medical Officer is the term given to a Specialist that contracts their services to a hospital. There are various ways that this occurs but lets stick with the most common one which is a sessional rate which is paid on an hourly basis.
Again sticking with NSW, a senior surgeon on a sessional VMO contract will earn $234.75 per hour plus $46.55 for background practice costs. That’s $281.30 per hour.
Were that surgeon to work 40 hours per week, just for the hospital for 48 weeks a year. That amounts to $540,096 AUD per annum. So about $80,000 more than what one could possibly earn as a Staff Specialist.
Of course, VMOs don’t generally just work for the public hospital system. They often consult from rooms and work in private hospital settings where they can generate greater revenue.
But to bring it back to reality a little bit. Working as a contractor means that you are not paid for your leave. You do not receive a professional development fund. And you have to carry your own Indemnity Insurance.
How Much Do Specialists Make Working in the Private Sector?
This question is a little bit more difficult to answer. Because there are no real reliable sources of information other than the broad information provided by the Australian Tax Office.
In addition, different specialists do different things. Some solely or primarily work in rooms, for example many Psychiatrists, General Practitioners and Physicians. Others work between rooms and hospitals, including most Surgeons and Anaesthetists.
Even the costs of running rooms can be considerable. Psychiatrists tend to have the lowest costs as they generally just need a comfortable office, reception and waiting room and a small amount of equipment. Versus, for example, Obstetricians and Gynaecologists who need a large amount of equipment to perform their job in rooms.
As we have also mentioned once you are in the private sector you are not just earning you are paying out expenses, which includes your own wage as well as the staff you employ, rent, various insurances, your own costs of professional development.
Also, when you go on leave you don’t get paid. But your staff generally do.
That being put aside we can do some rough estimations.
I’m going to use my own background specialty of Psychiatry for a simple example.
Lets say I work as a Psychiatrist solely in private rooms and charge patients for either half hour or 1 hour sessions. If I apply Australian Medical Association rates (which most specialists in private do). And I saw 4 patients for an hour and 8 patients for a half hour every day for 5 days a week for 47 weeks of the year (4 weeks leave and some adjustment for public holidays).
I would generate around $3,100 AUD in fees per day OR about $730,000 AUD per annum. This could go up somewhat if I charged for different items OR engaged in writing medico-legal reports.
This seems a lot and its and it is. And it doesn’t take into account all the costs I mentioned above.
For Specialists who are able to charge for procedures. Earnings scale up even more significantly. It is certainly not inconceivable therefore to see how some Surgeons in particular are making more than $1million per annum
Related Questions.
Question: How long does it take to become a Specialist in Australia?
Answer. A long time.
First, you need to go to medical school which is generally a minimum of 5 years for an undergraduate program. After graduating you then complete one or two provisional years which are called intern and resident years. You then apply for specialty training which in some cases is quite competitive (for example surgery) and therefore may take several years to get in. Most specialty training is a minimum of 5 years. Although General Practice training can take as little as 3 years.
So from entering into medical school to becoming a specialist may take you a minimum of 9 years but is more likely to take you about 12 or more.
For part of this time you are at medical school, incurring debt and with limited scope to work. But as we have pointed out above once you enter the hospital system you start to earn a decent wage helping you to pay off those debts. As a trainee you are probably already in the top ten of earners in the country. But you will have significant costs in terms of paying for your training. Exam fees and College fees tend to be in the several thousands of dollars. And you will be making this money partly due to working long hours.
Question: How much tax do Specialists pay?
Answer. This obviously depends on the Specialist and how much they earn. In Australia there are quite a few deductible expenses. So doctors are generally able to deduct things like equipment, insurance, college and exam fees, medical board fees even sometimes travel and accomodation. This will reduce the taxable income somewhat. Also many doctors who work privately will establish companies or trusts through which they collect some of their earnings. They may leave some of this money in these entities paying a lower corporate tax on the profits than if they were to pay themselves.
If we create an example of a full time Senior Staff Specialist in NSW who is not earning additional from their private billings. And has $20,000 in deductible expenses. They will have a taxable income of $296,891. Assuming that they have already cleared their university debts and have private health insurance, so don’t need to pay a medicare levy. Such a doctor would pay $106,860 in tax.
Question: How many doctors pay tax?
Answer. A fun fact is that if you count up all the doctors who filed a tax return according to the ATO figures there were 80,482 tax returns filed by doctors in 2016/17.
This post was compiled with acknowledgement to the Australian Taxation Office for some of the information in this post.
-

Career Coach Melbourne. How to Find a Good One & 4 More Tips
Career coaching is something I write about often. And there is a reason. Career coaching is something many professionals don’t give enough importance to. The truth is that a lot of people, especially medical professionals, can use career coaches to kick start or even keep their professional lives moving forward. This even includes medical students who are just entering the job market, as well as seasoned medical professionals looking to manage or make changes to their careers.
A good career coach can come from a range of backgrounds so long as they can help you fulfill your potential. They should also be able to understand your career needs, have achieved good outcomes for past clients and be someone you are comfortable with challenging you. If you are looking for a career coach in Melbourne there are plenty of good options. Some good general career and executive coaches include: Katie Roberts, Tenfold Coaching, Michelle Pizer and Noted Careers Coaching. For doctors specifically there is Jocelyn Lowinger of Coach GP. But you should also consider that there may be other good coaches that are a good fit for you elsewhere.
Limiting your search just to Melbourne may not necessarily be the smartest thing to do these days especially with online video technology. I will explain why later in this post.
But first in order to determine who might make a good career coach we need to know what one does.
Tip 1. Know What Makes a Career Coach
When we think about coaches we often think about sports coaches. And it’s a reasonable metaphor to start with. One way of looking at is that a coach simply takes you from one point to another, just like a bus. But at the end of the day, you have to determine what your destination will be. This is where the parallel with sporting coaches and career coaches tends to differ. Often in sports, the destination is reasonably clear, for e.g. make the finals, improve my time for the hundred metres. For careers, it may be clear, for e.g. get into surgical training, or not so clear, for e.g. do I want to take on a managerial position? That is why career coaches are so important. We spend a lot of our time working, and the truth is that a few major adjustments to our career lives can make huge differences to our professional and personal futures.
For instance, imagine the impact of completing your specialty training earlier could have on your annual salary and lifestyle. or how a different career leaves you with more time to spend on personal matters which could do to help you build a closer family?
Paying a career coach to help you fast track your career or make career changes and adjustments can be a very smart investment when it results in a significant boost to your income or helps you to meet other important goals.
Generally speaking, a career coach should help you find greater fulfillment in your profession and help you have the dream life you want to make out of your career. Let’s face it, for most people, the lives we dream of living depend substantially on the careers we have. Coaches can also help those looking for jobs, and ensure that those using their services do the best they can to fulfill their most cherished career goals.
Tip 2. How to Find A Career Coach.
Now that you have made the decision to invest in a career coach. Getting the right fit is very important for you. A coach who has achieved wonderful results with one person might not necessarily help you attain a similar level of success as your coach. Therefore, here are some tips for finding a good career coach.
1. Don’t consider their field, but their potential to help you achieve your goals
As you look for a career coach, it is important to remember that he/she does not have to be an expert at your specific field. So, if you are a surgeon, you do not have to focus on finding a career coach with a background in surgery. Similarly, for any doctor nderstand that there are lots of coach without a medical background who can help you.
The most important thing as you look for a career coach is to find someone who will inspire you and help you achieve your potential. A career coach should help you ask yourself thought-provoking and actionable questions that help you attain a particular career goal. A good career coach should also offer guidance and empower you to take appropriate action so that your career keeps moving forward.
2. Find someone who understands your career guidance needs
As you look for a career coach, you have to understand what your expectations are as far as these services go. You should try to work out beforehand what outcomes you expect out of the assistance the coach offers. So, whether you want a better paying job, or a more fulfilling career, or a different career path, you have to understand what kind of assistance you need.
That being said. If we knew exactly what we wanted. We might already know how to get there and not need a career coach. So a good career coach will also spend time with you to truly clarify your goals. Sometimes clients enter into career coaching with goals in mind that are really not their own goals but other peoples goals. Career coaches can help to clear up goal confusion.
Otherwise, if there is no clear focus on what your career goals are, a coach can also help you out with this. From there, find out what the career coach you are evaluating promises to help you achieve and see if it matches the specific career goals you have in mind.
3. Look into what they have achieved in the past
You can also have a look at their coaching bios and find out what former clients have to say of their skills. For instance, have the coaching skills helped someone in your specific field get what they wanted? Also consider their experience, because someone who is just entering the field might not be in a position to help you navigate an important career obstacle.
4. Choose someone you are comfortable with
How you feel about your career coach should also matter. You should trust your intuition based on the conversation you have with the coach. If for some reason you have doubts about their abilities to help you with your career, then it’s worth looking at what other career coaches have to offer.
At the end of the day, you should have a great rapport with your career coach. This is important because however successful the coach has been in the past with former clients, he/she might not be the best fit for you if your strained relationship gets in the way of their offering you sound career guidance.
You should not just go and book sessions with the first coach you find with the expectation that your career will be changed for the better. Consider making a quick call with them first. Most good coaches will offer a quick free call service because they are confident in their abilities and they know this helps clients to make a decision about their services.
Tip 3. Investigate How a Career Coach in Melbourne Costs.
There is no particular standard by which career coaches in Melbourne or other parts of Australia fix their rates. Career coaching is essentially a free market. You will generally be getting what you pay for. If a career coach sets a high rate it is generally because their clients see the sort of results from their coaching to pay that rate.
Bear in mind that when you are paying for an hour of coaching you are probably not just paying for the coaches direct time. They will have administrative costs to factor in and possibly support staff, insurances, rent, website etc… They will also likely be doing some work for you outside of the session, such as researching issues, setting up for the next session and responding to emails from you.
In Australia, most basic level career coaches will charge at least $150 for a one-hour session. Some may provide discounted rates depending on your ability to pay. These coaches tend to be more targeted to younger people just entering the job market and might not have the experience and expertise to work with the majority of medical practitioners who already have a developed career.
Mid-range career coaches will charge somewhere between $300-600 AUD per session. These are the types of coaches who tend to work with most doctors.
An elite level career coach in Melbourne may charge $1,000 or more a session. If you are working as a medical Executive or CEO you might be able to afford the services of such a coach.
As I mentioned most coaches will provide a discount based upon your ability to pay. They may also pay a discount if you purchase a package of coaching. Sometimes you need to ask about this. It never hurts to do so.
Several factors come into play as far as career coaching goes. including, how long you will work with the professional, as well as the complexity of the goal you are trying to attain. Obviously, if you want help getting starting a career in a specialty with high barriers to entry, you might expect to need more sessions and pay a bit more than someone who just needs once off help preparing for an upcoming job interview.
It is important to remember that each career coach will charge you different fees for the same types of services. So, even as you try to find a bargain, it is important to remember that you will generally get what you pay for.
If you want cheap services, then you might end up getting poor quality services as well. Generally, coaches who have been in the business for much longer can and do charge more, and that because they are usually more successful at helping their clients achieve their career goals. This assurance obviously comes at a premium. But you will probably also find that because you are paying more they are actually seeing fewer clients and will give you extra support outside of the formal coaching sessions.
That said, you can always negotiate with your career coach so that you get a price that you can handle. However, what your career coach has to offer also matters. For instance, if they have a vast professional network that can provide you with other forms of career assistance, then you can expect to pay more. As opposed to coaches who will only stop at helping you polish up your interview performance.
Tip 4. Understand What a Career Coach Does.
Career coaches can do plenty to assist you to accomplish your career goals. Some of the things they can help you out with include the following.
- Showing you how to deal with office politics
- Help you understand yourself, your career strengths, and what value you can offer
- Guide you on resolving feelings like frustration, anger, and resentment with regard to your current job
- Help you meet with more success at work
- Help you to manage difficult conversations and difficult team dynamics at work
- Help you to get better feedback on your performance at work
- Help you to manage your relationship with your boss
- Help you to manage your relationship with your co-workers
- Help you be a better manager, if your role involves managing
- Show you how to land your dream job or career
- Guide you towards your most appropriate career based on your skills and interests
- Assist you in planning, developing and managing your career path
- Help you recognize things that are stressing you at work and helping you deal with them
- Help you identify problems that affect your career and satisfaction as a professional
- Helping you find more passion in what you do when you are stuck in a rut
- Helping you to make a difficult decision about exiting your current career
It is important to realize that a career coach is there to assist you, which means you have to play your part as well. At the end of the day, you have to work towards becoming what you want as far as your professional life goes and resolving any career issues you might be facing. Essentially, they use their training, experience, expertise and skills to help you overcome hurdle that keep most people from becoming all they would like to be. Otherwise, these professionals are also restricted by other factors, including your qualifications, your attitude, and how well you are willing to work with them.
Conclusion.
At the end of the day, you can think of a career coach as an experienced friend who can help you achieve your dreams more easily or with greater chances of success. Once you know what changes you need to be making in your career, you should hire this professional to help you along. While at it, consider what the professional you have in mind can offer, how much it will cost you, and what assurances you have as far as delivering on their promises goes.
Related Questions.
Question: Who trains career coaches?
Answer.
The career coaching industry is not regulated. But some take courses, and others do it because they have enough experience in the corporate world to offer the much-needed guidance to people in search of the services require to resolve the career issues they are facing. There are some international organisations which some coaches belong to.
Question: How does career coaching work?
Answer.
Basically, the service involves talking through issues and ideas in order to get the services you desire as the client. If you want to land a dream job, you can get confidence building sessions to help you do better at things like interviews in addition to technical skills, such as how to write a killer CV. Sometimes there may be other activities performed by the coach for you, for example administering surveys on your behalf to get feedback on your impact at work.
Question: Does it matter if my career coach is in Melbourne or not?
Answer.
Some people think that where the career coach comes from matters a big deal. However, this is not always necessary, even if the desire is to have a face-to-face interaction with the career coach. In fact with technology these days it is incredibly easy to connect with a coach via video on your computer or even smart device. This actually offers up a few advantages.
Firstly, it potentially expands the range of coaches you may be able to engage with.
Secondly, it often makes scheduling appointments easier as the coach is not pinned down to meeting you in a certain office or location at a certain time.
Thirdly, it means you are not having to travel somewhere to see the coach.
Fourthly, the sessions can often be recorded and provided back to you to review.
-

GP Training How To: Pathways, Length, Difficulty & Options for IMGs
Dr Rebecca Stewart guest blogs for us on an important question. Rebecca is a GP and Medical Educator who is passionate about supporting competence and excellence in medical education, research, and evaluation. Rebecca provides individualized support for GP training, including GPs attempting Fellowship examinations and has developed a suite of study resources, including the first research and curriculum-based study planning App for Australian General Practice visit MedEd ExpertsBegin with the end in sight: Pathways in Australian General Practice.
Writing this blog was a hard slog. Navigating through the intricacies of working in Australian General Practice must be one of the most confusing and disorientating journeys I’ve ever been on – and I have been trained and work in Australian General Practice! I cannot imagine how a trainee doctor or a doctor from overseas who is less familiar with the environment would find their way without some guidance. So I hope in writing this blog as an expert I can make your journey to working independently as a GP in Australia a little smoother.
Before we get too much into the detail. Let’s answer the key question here. How can overseas trained doctors (International Medical Graduates) work in General Practice in Australia? The short explanation is that you firstly need to be assessed for and given registration to work in a general practice position. As a minimum this requires you to have passed the AMC Part 1 Exam and meet the AHPRA requirements for English. You also need a job offer with appropriate supervision. At this point there are various options under what is called the 3GA position to work in a post in general practice where you can offer Medicare services.
The road to GP Fellowship can be long and tortuous and requires considerable personal and academic commitment – so before you set off, plan your route to ensure a straight trajectory. Many of the doctors that I work with in preparation for (and/or repeatedly attempting) Fellowship exams started their ‘trip to Fellowship’ late. Or stumbled along the path. Repeatedly finding hazards, including AHPRA Registration hurdles.
Working independently in General Practice should be enjoyable and challenging and doesn’t have to be tortuous.
Some Initial Questions to Ask Yourself.
Before you embark on your journey into General Practice in Australia ask yourself the following questions:
- Where do you wish to be working in five years? I.e. what type of medicine would you like to practice and what skillsets will you need?
- Are you subject to 19AA or 19AB legislation? Otherwise known as Vocational Registration and the Moratorium
- Are you here on a Visa or are you a permanent resident?
- Do you want to work in an urban or rural area?
- Can you afford to self-fund your General Practice training?
- Are you working under any AHPRA registration restrictions?
- Can you afford to work under A1 or A2 rebates?
If you’re not sure what these questions are about then this blog is definitely for you and you should read on.
There are two key concepts that need to be considered. The first is working in General Practice. The second is the training and assessment required to be undertaken in order to achieve a GP Fellowship.
If you intend to stay living and working in Australia in General Practice in the long term then you both need a job as well as a Fellowship.
Working in General Practice.
To work in Australian General Practice, you need to be able to access Medicare for your patients.
An explanation of Medicare deserves its own blog post. But for now the basic thing you need to understand is that in Australia there is a system of universal health insurance which funds by far the majority of health services in Australia, this includes both community provided services as well as hospital services. All Australian citizens and permanent residents are covered under this scheme. In addition a number of other people living in Australia whose governments have reciprocal arrangements with Australia are also covered under Medicare.
The Australian Government provides funding for services by way of rebating items which doctors are able to charge for. These are called Medicare items.
If you are not able to charge for Medicare in General Practice you are at a serious disadvantage as most patients will not be able to afford to see you or will choose to go see a GP who can access Medicare.
There are two levels of rebates available for GPs. A1 which entitles the patient to 100% of the rebate, and A2 where the patient can only claim 80% of the Medicare rebate.
Medicare Provider Numbers.
To access Medicare you need a Medicare Provider Number. A Provider Number is required for each place of practice and profession your practice in. Provider numbers are available by filling in a form , or through Provider Digital Access/PRODA .
Doctors in Australia are not automatically eligible for a provider number. You are only eligible for a Provider Number if:
- You are a recognised specialist, which the government divides in to General Practitioner and consultant physicians (basically all other specialists); OR
- You are in an approved placement under 3GA (see below) of the Health Insurance Act 1973 ; OR
- You are a temporary resident doctor with an exemption under section 19AB of the Health Insurance Act 1973 and working in accordance with that exemption.
Why Do You Need a Provider Number?
A bit of background is required in order to answer this question. In 1996, Section 19AA of the Health Insurance Act was introduced to recognise General Practice as a vocational specialty in its own right. Prior to this any doctor with General Registration could set up shop as a General Practitioner and charge for General Practice items under Medicare. After 1996 a system of Vocational Registration was introduced, whereby doctors now need to demonstrate (generally through gaining a Fellowship) that they are qualified to work as a general practitioner.
Doctor’s subject to Section 19AA are:
- Those doctors who attained Australian Medical Board registration on or after 1/11/96; and
- Permanent residents; and
- Those doctors who do not hold continued recognition with the Royal Australian College of General Practice (RACGP) or Australian College of Rural and Remote Medicine (https://www.acrrm.org.au/).
You gain continued recognition with the RACGP or ACRRM by either completing their Fellowship requirements or having been “grandfathered” into either College prior to 1996.
So basically, whilst there are some doctors who can gain an exception to 19AA or Vocational Registration. These doctors are slowly dwindling in number over the years.
What Happens If You Are Not Vocationally Registered?
Any doctor who is not vocationally registered must be on what is called an approved 3GA program in order to access Medicare Benefits. This is regardless of whether this doctor has trained in Australia or overseas.
Your 19AA restriction ends when you attain recognition (Fellowship) with a specialist college.
For more information about this, see this Fact Sheet .
3GA Programs.
To enable access to a Provider Number and ensure your patients receive 100% of the Medicare rebate, working within a 3GA program is essential.
You also have to take into account any 19AB requirements (which may restrict you to working in certain areas of workforce shortage).
You can change from one 3GA program to another but your cannot be on programs simultaneously.
These are more than 9 3GA programs. So it can be quite confusing which one to apply for and which one is best.
IMG doctors who have completed their AMC Part 1 and satisfy the AHPRA English requirements are able to apply for most of the 3GA programs listed below. So long as they have an offer of employment and suitable supervisory arrangements.
However, in my experience it can be challenging to go through both the AMC process and work in general practice. So it may be better to focus on getting yourself up to general registration first, obtaining permanent residency and then commencing general practice training via the main 3GA program the Australian General Practice Training Program.
Lets start with the main one.
The Australian General Practice Training Program.
The Australian General Practice Training Program is a key 3GA program and the main pathway for doctors trained in Australia to enter into training in general practice and charge for Medicare items whilst undertaking their training.
It is also a pathway for any IMG who may obtain general registration through the Standard Pathway process by completing the requirements for the AMC Certificate and a year of supervised practice.
Under the Australian General Practice Training Program (AGPT):
* You can train towards Fellowship with RACGP or ACRRM
* You can apply for either general or rural streams. For most IMG doctors you will have to apply for the rural stream as you will be restricted to areas of District of Workforce Shortage.
* Applications open in April each year.
* There is a Selection process
* And Eligibility Criteria
* Training year commences in JanuaryThe AGPT is Commonwealth Government funded and includes comprehensive in-practice supervision and training, and external education supports including resources, workshops and Medical Educator support.
The costs for undertaking the program are nil to low.
There are 1350 places for AGPT under the RACGP and 150 places under the ACRRM each year.
The RACCGP Practice Experience Program.
The RACGP Practice Experience Program (PEP): is a self-directed education program designed to support non-vocationally registered (non-VR) doctors on their journey to RACGP Fellowship. To be eligible to apply you have to demonstrate that you have a significant level of prior experience in general practice in Australia. The program is currently a 12 – 18-month program with a mid and end of year intake. It includes education resources and Medical Educator feedback and support.
The program costs the applicant $2,000 per 6 months and there is some Commonwealth funding support.
See here for the Eligibility criteria for this program.
ACRRM Independent Pathway.
The ACRRM Independent Pathway is similar in nature to the AGPT program in both application and structure. However, there is more flexibility in location and no streaming in the program. The program is designed to address areas of workforce shortage by supporting applicants in such positions. There are prior experience requirements and you need to self-fund your participation (approximately $30,000 in total).
It is possible to do a procedural/advanced skill component as part of the program.
Here are the Eligibility criteria for the program.
ACRRM Non-Vocationally Registered Support Program
The ACRRM Non-Vocationally Registered Support Program is similar to the ACRRM Independent Pathway. With the main difference being that there is up to $15,000 Commonwealth support provided.
Rural Locum Relief Program.
The Rural Locum Relief Program (RLRP) aims to ensure that Australian rural and remote communities have access to appropriately experienced and skilled medical practitioners.
The RLRP allows medical practitioners, in rural and remote areas who are subject to Section 19AA of the Act and who meet eligibility criteria of the program, to have temporary access to Medicare rebates when providing short term services through approved placements.
Eligibility
Applicants eligible for the RLRP fall into two broad categories:
- Category 1 applicants: Australian and New Zealand graduates, Australian Citizens and Permanent Resident Overseas Trained Doctors (OTDs) who are subject to Section 19AA of the Act only
- Category 2 applicants: Australian Citizens, Permanent Resident OTDs and foreign graduates of an accredited medical school who are subject to both Sections 19AA and 19AB of the Act (the ten year moratorium)
You need two years prior GP experience for the RACGP pathway. The amount of time you can spend on the program differs in length in each State and territory but is 2-4 years on average. Its quite a flexible program. And probably has to be given that you are moving around doing locum jobs. For each placement you need an onsite VR mentor and you have to be be working in a rural area. (RRMA 3-7 for the technical specifics). There is minimal structure. The only real support is a mentor.
Under the Rural Locum Relief Program it is possible to sit either the RACGP or ACRRM Fellowship exams. And there is funding support for doctors to sit these exams.
The Remote Vocational Training Scheme.
Under the Remote Vocational Training Scheme (RVTS): doctors can train towards FRACGP or FACRRM. You must be working in a rural area or Aboriginal Medical Service
The scheme requires a minimum of 2 years GP experience in the practice you are working in
This is a well-structured and funded program with remote supervision and external Medical Educator support and resources.
Go here for the Eligibility criteria
More Doctors for Rural Australia Program.
The More Doctors for Rural Australia (MDRAP) Program enables access to Medicare before you transition to a college program.
After Hours Medical Deputising Program.
Under the After Hours Medical Deputising (AMDS) Programs :
you are able to train towards RACGP or ACRRM Fellowships. You can work in both metropolitan and regional areas, in clinics or home visits.All work is after-hours: 6 pm – 8am weekdays, Saturday after 12, Sunday and public holidays.
An interesting component of this program is that higher billing rates are possible in some after-hours segments.
However, your experience under this program is assessed at 50% of the actual time worked as after hours deputising is not considered comprehensive and holistic general practice and is capped at 2.5 years.
Your limited scope of practice can also make it more difficult to contextually apply knowledge for Fellowship exams.
Special Approved Placement Program.
The Special Approved Placement Program (SAPP) :is a program for doctors with extenuating circumstances. Its main aim is to assist doctors to become eligible for another program.
Other Programs.
There are a range of other programs available, however, the Commonwealth Government has signalled that they will be phasing most of these out in the not too distant future.
- Approved Private Emergency Department Program (
ADEDP ) - Approved Placements for Sports physicians Program (APSPP)
- Sports Physician Trainees Program
- Prevocational General Practice Training Program (outdated)
- Queensland Country Relieving Doctors Program
- http://www.health.gov.au/internet/main/publishing.nsf/Content/work-pr-ompsOther Medical Practitioners (OMPs) programs
No new participants are being admitted to these programs after 1/11/18 and existing participants will have five years to attain Fellowship or will be moved to less favourable rebates.
With So Many 3GA Schemes It Couldn’t Possibly Go Wrong. Could It?
Yes it can. And frequently. As noted above your time on these schemes is generally limited and aimed at you progressing towards a fellowship.
Here’s a case example to illustrate the point.
Dr X is an IMG who works in a small rural town. He has gained permanent residency, and is therefore subject to Section 19AA of the Health Act, and is an IMG so also subject to Section 19AB. He has a Provider Number through the Rural Locum Relief Program and was enrolled to sit Fellowship exams which he has attempted multiple times, but due to personal circumstances had to withdraw at the last minute. In the meantime, his AHPRA Registration requires renewal, including evidence of progression towards Fellowship, which due to exam withdrawal is now problematic. He is currently not eligible to enrol for the next exam cycle due to a likely lapsed Medical Board Registration, which is required for enrolment. This is a common example of the complexities of the system and the need to ensure that you have a good understanding of all of the factors for both working and training in General Practice.
What Is a District of Workforce Shortage?
Section 19AB of the Health Insurance Act requires Overseas Trained Doctors (OTDs) and Foreign Graduates of Accredited Medical Schools (FGAMS) to practice in an area of District Workforce Shortage for ten years after their first Australian Medical Board Registration.
Whilst many doctors think that this means you will be consigned to a very remote or rural location for ten years. This is often not the case as many parts of the larger cities in Australia are considered to be areas of District of Workforce Shortage.
If you want to visualise this concept you can pop over to the highly helpful doctor connect website.
Exemptions and reductions in the ten year moratorium are available in some cases to this requirement. For more information, see this Fact Sheet .
Training in General Practice.
Vocational registration is attained with Fellowship of either the RACGP or ACRRM. There are significant differences in these programs. So its worth investigating both options before you decided which one is best for you.
Phasing Out of 3GA Programs.
The Commonwealth has indicated that by 30 June 2023 many of the existing 3GA programs will be phased out. Doctors will need to attain Fellowship or join a college-led Fellowship training Program to maintain A1 rebates.
Let’s make an itinerary.
Your route may seem complex. The following diagram is aimed to assist you in reviewing all the options available to you.
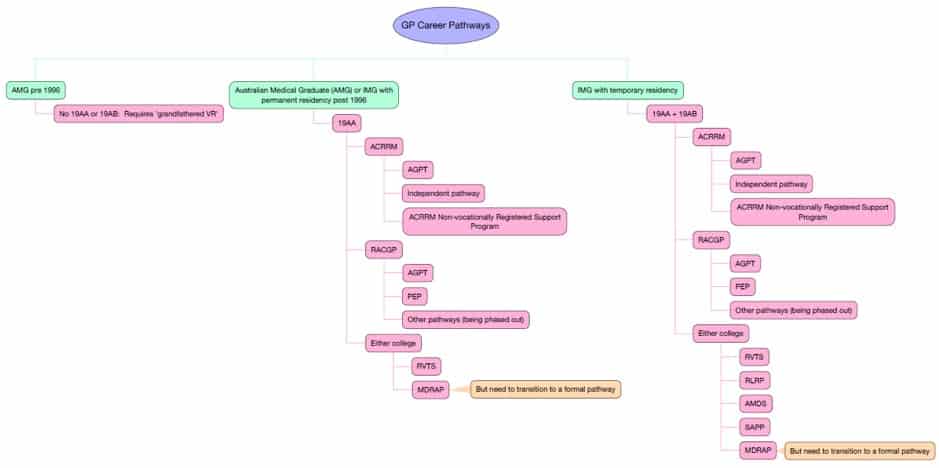
GP Career Paths The options have been simplified to provide guidance so please revise all eligibility criteria prior to planning your approach. View a pdf of the flowchart here.
Destination Fellowship.
Vocational Registration is given to work in General Practice when you have attained a Fellowship with the RACGP or ACRRM.
The eligibility for each exam depends on your previous experience in General Practice and what pathway you are on. Check the RACGP and ACRRM exam eligibility for your individual circumstance.
The assessment and Fellowship for the two colleges differ considerably (see table below). ACRRM Fellowship also requires completion of an Advanced Skill (for e.g. Anaesthetics, Obstetrics). Advanced Skills can also be completed as part of a Fellowship of Advanced Rural General Practice (FARGP) with the RACGP.
RACGP Assessments include:
- Applied Knowledge Test (AKT)
- Key Features Paper (KFP)
- Objective Structured Clinical Examination (OSCE)
ACRRM Assessments include
- Procedural Logbook
- MCQ
- Multi-source Feedback
- Case Based Discussion
- Structured assessments using multiple patient scenarios (StAMPS)
- Advanced Skill Assessments – StAMPS and/or a Project
One you have decided that GP is the career for you, it is not only critical to ensure you are on the right pathway, but to map out when you might complete the Fellowship assessments. Many of the doctors that I work with underestimate the degree of difficulty of the assessments. Some sit the exams without adequate preparation as either they ‘will just give it a go to see what it’s like’ or they are pressured to sit due to other factors including AHPRA Registration requirements.
An unsuccessful exam attempt usually impacts upon personal and professional confidence and makes a huge hole in your hip pocket. RACGP has recently introduced a capping on exam attempts and ACRRM has a strict policy regarding multiple attempts so it is better to plan for success in the first instance.
Do I need a Trip Advisor?
If you’re deciding on what journey to take in medicine, Dr Anthony Llewellyn is an experienced health public sector executive, medical educationalist and coach. Contact him at AdvanceMed .
If you’ve already headed a little way down the Fellowship path (any speciality) and are feeling a bit lost, then a chat with Dr Ashe Coxon at Medical Career Planning might help. Dr Coxon is a GP, Medical Educator and Medical Career Consultant.
If trudging down the GP Fellowship road, then Medical Education Experts is here to support your journey with individualised coaching and learning resources . We have a MAP , a GPS System and a Compass that will keep you on track when planning your study for exams.
Its More Fun To Travel In a Group.
Find some colleagues to enjoy the ride with, and if you’re feeling a bit lost and confused, ask for some professional advice.
Useful Resources and Links:
- 19AA and the 3GA Program s
- DHS Changes to 3GA programs
- Doctor Connect: DWS locator
- Doctor Connect: Working as a GP
- Medicare benefits for health professionals, intern, registrar and trainee eligibility requirements .
- Other Medical Practitioners (OMPs) programs .
- PESCI Information for IMGs
- RACGP Practice Experience Pathway
- Section 3GA programs
- Stronger Rural Health Strategy – Streamlining General Practice Training
- Training – improved access to Australian trained general practitioners and quality care
Related Questions.
Question: What is General Practice?
Answer.
In Australia General Practice is considered to be its own medical specialty. In other countries this specialty might be referred to as either family medicine or primary care medicine.
According to the RACGP in Australia, a GP:
- is most likely the first point of contact in matters of personal health;
- coordinates the care of patients and refers patients to other specialists;
- cares for patients in a whole of person approach and in the context of their work, family and community;
- cares for patients of all ages, both sexes, children and adults across all disease categories;
- cares for patients over a period of their lifetime;
- provides advice and education on health care
- performs legal processes such as certification of documents or provision of reports in relation to motor transport or work accidents.
Question: Can I Be On More Than One 3GA Program At a Time?
Answer.
No. You can change from one 3GA program to another but your cannot be on programs simultaneously.
Question: What Happens After I Complete 10 Years In a District of Workforce Shortage?
Answer. Basically you are now free to work anywhere you chose in Australia. Its likely by this point that you will also have been able to apply for permanent residency and even citizenship. So you will essentially be the same as every Australian born and trained GP.
-

Career Coach. When Do You Need One? Costs & How to Find a Good One.
Being a success at what you do is a great feeling. This is why you need all the help you can to get to this point. On our blog, you will find a lot of tips and information on how to make the best of your medical career. Put together by an experienced team of doctors, this blog contains the critical information you need to manage your medical career and achieve your greatest career goals as a doctor in Australia. And is also helpful for other parts of the world.
Career coaching is something I write about often. And there is a reason. Career coaching is something many professionals don’t give enough importance to. The truth is that a lot of people, especially medical professionals, can use career coaches to kickstart or even keep their professional lives moving forward. This even includes medical students who are just entering the job market, as well as seasoned medical professionals looking to manage or make changes to their careers.What is a Career Coach?
When we think about coaches we often think about sports coaches. And it’s a reasonable metaphor to start with. One way of looking at is that a coach simply takes you from one point to another, just like a bus. But at the end of the day, you have to determine what your destination will be. This is where the parallel with sporting coaches and career coaches tends to differ. Often in sports, the destination is reasonably clear, for e.g. make the finals, improve my time for the hundred metres. For careers, it may be clear, for e.g. get into surgical training, or not so clear, for e.g. do I want to take on a managerial position? That is why career coaches are so important. We spend a lot of our time working, and the truth is that a few major adjustments to our career lives can make huge differences to our professional and personal futures.
For instance, imagine the impact of completing your specialty training earlier could have on your annual salary and lifestyle. or how a different career leaves you with more time to spend on personal matters which could do to help you build a closer family?
Paying a career coach to help you fast track your career or make career changes and adjustments can be a very smart investment when it results in a significant boost to your income or helps you to meet other important goals.
Generally speaking, a career coach should help you find greater fulfillment in your profession and help you have the dream life you want to make out of your career. Let’s face it, for most people, the lives we dream of living depend substantially on the careers we have. Coaches can also help those looking for jobs, and ensure that those using their services do the best they can to fulfill their most cherished career goals.
How to Find A Career Coach.
Now that you have made the decision to invest in a career coach. Getting the right fit is very important for you. A coach who has achieved wonderful results with one person might not necessarily help you attain a similar level of success as your coach. Therefore, here are some tips for finding a good career coach.
1. Don’t consider their field, but their potential to help you achieve your goals
As you look for a career coach, it is important to remember that he/she does not have to be an expert in your specific field. So, if you are a surgeon, you do not have to focus on finding a career coach with a background in surgery. Similarly, for any doctor understand that there are lots of coaches without a medical background who can help you.
The most important thing as you look for a career coach is to find someone who will inspire you and help you achieve your potential. A career coach should help you ask yourself thought-provoking and actionable questions that help you attain a particular career goal. A good career coach should also offer guidance and empower you to take appropriate action so that your career keeps moving forward.
2. Find someone who understands your career guidance needs
As you look for a career coach, you have to understand what your expectations are as far as these services go. You should try to work out beforehand what outcomes you expect out of the assistance the coach offers. So, whether you want a better paying job, or a more fulfilling career, or a different career path, you have to understand what kind of assistance you need.
That being said. If we knew exactly what we wanted. We might already know how to get there and not need a career coach. So a good career coach will also spend time with you to truly clarify your goals. Sometimes clients enter into career coaching with goals in mind that are really not their own goals but other peoples goals. Career coaches can help to clear up goal confusion.
Otherwise, if there is no clear focus on what your career goals are, a coach can also help you out with this. From there, find out what the career coach you are evaluating promises to help you achieve and see if it matches the specific career goals you have in mind.
3. Look into what they have achieved in the past
You can also have a look at their coaching bios and find out what former clients have to say of their skills. For instance, have the coaching skills helped someone in your specific field get what they wanted? Also consider their experience, because someone who is just entering the field might not be in a position to help you navigate an important career obstacle.
4. Choose someone you are comfortable with
How you feel about your career coach should also matter. You should trust your intuition based on the conversation you have with the coach. If for some reason you have doubts about their abilities to help you with your career, then it’s worth looking at what other career coaches have to offer.
At the end of the day, you should have a great rapport with
your career coach. This is important because however successful the coach has been in the past with former clients, he/she might not be the best fit for you if your strained relationship gets in the way of their offering you sound career guidance.You should not just go and book sessions with the first coach you find with the expectation that your career will be changed for the better. Consider making a quick call with them first. Most good coaches will offer a quick free call service because they are confident in their abilities and they know this helps clients to make a decision about their services.
How Much Does a Career Coach Cost?
There is no particular standard by which career coaches fix their rates. Career coaching is essentially a free market. You will generally be getting what you pay for. If a career coach sets a high rate it is generally because their clients see the sort of results from their coaching to pay that rate.
Bear in mind that when you are paying for an hour of coaching you are probably not just paying for the coaches direct time. They will have administrative costs to factor in and possibly support staff, insurances, rent, website etc… They will also likely be doing some work for you outside of the session, such as researching issues, setting up for the next session and responding to emails from you
. In Australia, most basic level career coaches will charge at least $150 for a one-hour session. Some may provide discounted rates depending on your ability to pay. These coaches tend to be more targeted to younger people just entering the job market and might not have the experience and expertise to work with the majority of medical practitioners who already have a developed career.
Mid-range career coaches will charge somewhere between $300-600 AUD per session. These are the types of coaches who tend to work with most doctors.
An elite level career coach may charge $1,000 or more a session. If you are working as a medical Executive or CEO you might be able to afford the services of such a coach.
As I mentioned most coaches will provide a discount based upon your ability to pay. They may also pay a discount if you purchase a package of coaching. Sometimes you need to ask about this. It never hurts to do so.
Several factors come into play as far as career coaching goes. including, how long you will work with the professional, as well as the complexity of the goal you are trying to attain. Obviously, if you want help getting starting a career in a specialty with high barriers to entry, you might expect to need more sessions and pay a bit more than someone who just needs once off help to prepare for an upcoming job interview.
It is important to remember that each career coach will charge you different fees for the same types of services. So, even as you try to find a bargain, it is important to remember that you will generally get what you pay for.
If you want cheap services, then you might end up getting poor quality services as well. Generally, coaches who have been in the business for much longer can and do charge more, and that because they are usually more successful at helping their clients achieve their career goals. This assurance obviously comes at a premium. But you will probably also find that because you are paying more they are actually seeing fewer clients and will give you extra support outside of the formal coaching sessions.
That said you can always negotiate with your career coach so that you get a price that you can handle. However, what your career coach has to offer also matters. For instance, if they have a vast professional network that can provide you with other forms of career assistance, then you can expect to pay more. As opposed to coaches who will only stop at helping you polish up your interview performance.
What Does a Career Coach Do?
Career coaches can do plenty to assist you to accomplish your career goals. Some of the things they can help you out with include the following.
- Showing you how to deal with office politics
- Help you understand yourself, your career strengths, and what value you can offer
- Guide you on resolving feelings like frustration, anger, and resentment with regard to your current job
- Help you meet with more success at work
- Help you to manage difficult conversations and difficult team dynamics at work
- Help you to get better feedback on your performance at work
- Help you to manage your relationship with your boss
- Help you to manage your relationship with your co-workers
- Help you be a better
manager, if your role involves managing - Show you how to land your dream job or career
- Guide you towards your most appropriate career based on your skills and interests
- Assist you in planning, developing and managing your career path
- Help you recognize things that are stressing you at work and helping you deal with them
- Help you identify problems that affect your career and satisfaction as a professional
- Helping you find more passion in what you do when you are stuck in a rut
- Helping you to make a difficult decision about exiting your current career
It is important to realize that a career coach is there to assist you, which means you have to play your part as well. At the end of the day, you have to work towards becoming what you want as far as your professional life goes and resolving any career issues you might be facing. Essentially, they use their training, experience, expertise, and skills to help you overcome hurdles that keep most people from becoming all they would like to be. Otherwise, these professionals are also restricted by other factors, including your qualifications, your attitude, and how well you are willing to work with them.
Conclusion.
At the end of the day, you can think of a career coach as an experienced friend who can help you achieve your dreams more easily or with greater chances of success.
Once you know what changes you need to be making in your career, you should hire this professional to help you along. While at it, consider what the professional you have in mind can offer, how much it will cost you, and what assurances you have as far as delivering on their promises goes.Related Questions.
Question: Who trains career coaches?
Answer.
The career coaching industry is not regulated. But some take courses, and others do it because they have enough experience in the corporate world to offer the much-needed guidance to people in search of the services required to resolve the career issues they are facing. There are some international organizations which some coaches belong to.
Question: How does career coaching work?
Answer.
Basically, the service involves talking through issues and ideas in order to get the services you desire as the client.
If you want to land a dream job, you can get confidence building sessions to help you do better at things like interviews in addition to technical skills, such as how to write a killer CV. Sometimes there may be other activities performed by the coach for you, for example, administering surveys on yourbehalf to get feedback on your impact at work.Question: Does the location of the career coach matter?
Answer.
Some people think that where the career coach comes from matters a big deal. However, this is not always necessary, even if the desire is to have a face-to-face interaction with the career coach. In fact with technology these days it is incredibly easy to connect with a coach via video on your computer or even a
smart device. This actually offers up a few advantages.Firstly, it potentially expands the range of coaches you may be able to engage with.
Secondly, it often makes scheduling appointments easier as the coach is not pinned down to meeting you in a certain office or location at a certain time.
Thirdly, it means you are not having to travel somewhere to see the coach.
Fourthly, the sessions can often be recorded and provided back to you to review.
